To get a real handle on arthritis pain, you need a plan that’s built for you. A truly effective strategy combines smart lifestyle adjustments, targeted exercise, and an anti-inflammatory diet with the right medical care. This isn’t just about chasing symptoms; it's about addressing the root causes to find lasting relief.
And the first, most critical step? Knowing exactly what kind of arthritis you're dealing with.
Understanding Your Arthritis Pain
Before you can build an effective management plan, you have to know your opponent. "Arthritis" isn't a single diagnosis. It’s an umbrella term for joint inflammation, and the source of your pain determines the best way to fight back.
The two most common types you’ll encounter are Osteoarthritis (OA) and Rheumatoid Arthritis (RA). They might share a name, but their origins—and how you treat them—are worlds apart.
Osteoarthritis vs. Rheumatoid Arthritis
Osteoarthritis is what many people call "wear-and-tear" arthritis. It happens when the slick, protective cartilage on the ends of your bones gradually wears down over the years. Imagine the tread on a tire getting thinner with every mile—that’s what’s happening in your joints. This eventually leads to bone rubbing on bone, causing a deep, aching pain that typically gets worse the more you move.
Rheumatoid Arthritis, on the other hand, is an autoimmune disorder. This means your own immune system gets confused and starts attacking healthy tissues, specifically the delicate lining of your joints called the synovium. This misguided assault triggers chronic inflammation, which leads to the pain, swelling, and stiffness you feel. RA pain is often symmetrical (affecting both wrists or both knees, for example) and is usually at its worst first thing in the morning.
The global impact of RA is growing. Research indicates that from 1990 to 2019, the prevalence of RA crept up by about 0.37% each year, with a significant jump of 14.1% by 2020. This underscores just how vital it is to combine pain management with treatments that address the disease itself.
Key Takeaway: Grasping this difference is everything. OA management is often about reducing joint stress and soothing symptoms. RA treatment, however, must also tackle the underlying autoimmune attack to prevent permanent joint damage.
To make this distinction clearer, here’s a quick comparison.
Key Differences Between Osteoarthritis and Rheumatoid Arthritis
This table offers a quick-reference guide to help you distinguish between the two primary types of arthritis discussed here.
| Feature | Osteoarthritis (OA) | Rheumatoid Arthritis (RA) |
|---|---|---|
| Primary Cause | Mechanical wear and tear on cartilage | Autoimmune disease attacking joint lining |
| Pain Pattern | Often asymmetrical (e.g., one knee) | Typically symmetrical (e.g., both wrists) |
| Morning Stiffness | Usually lasts less than 30 minutes | Often lasts longer than 30 minutes |
| Systemic Symptoms | None; confined to the joint | Can include fatigue, fever, and malaise |
| Onset | Tends to develop gradually over years | Can develop relatively quickly (weeks to months) |
| Treatment Focus | Pain relief, preserving function, exercise | Suppressing immune system, reducing inflammation |
Understanding these fundamental differences is the starting point for developing a truly effective and targeted management plan.
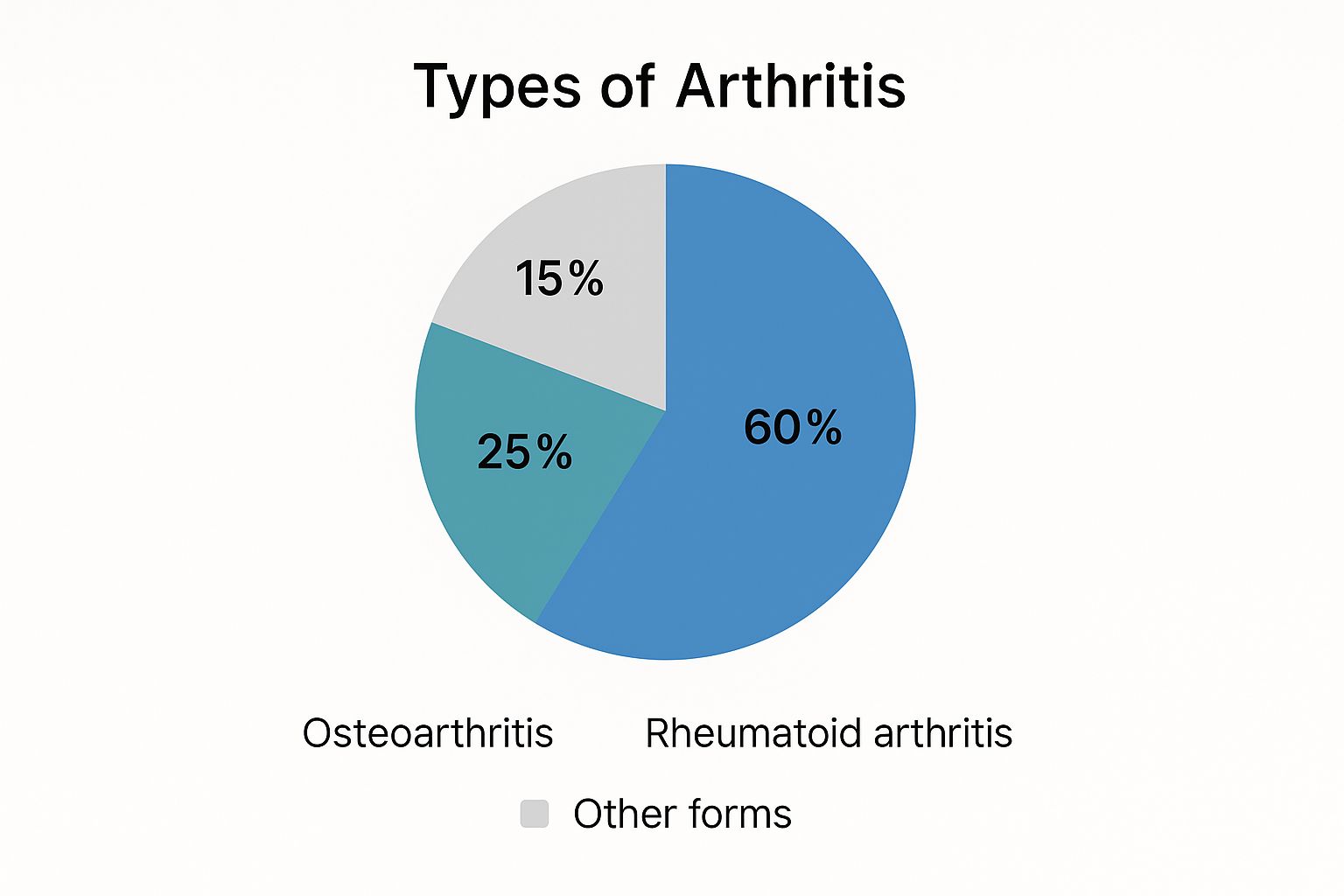
As you can see, Osteoarthritis is far and away the most common type, making it a major focus for countless people searching for ways to manage their pain. By pinpointing whether your pain is from mechanical wear or an autoimmune process, you and your doctor can craft a much smarter, more effective plan for relief.
Finding Relief Through Movement and Exercise

When your joints ache, the last thing you probably want to do is move. The natural instinct is to stay still and rest. While rest certainly has its place, especially during a bad flare-up, a complete lack of movement is one of the biggest myths when it comes to managing arthritis.
In my experience, the right kind of consistent exercise is one of the most powerful tools we have for long-term pain relief. Think of your joints like the hinges on a gate—if they’re never used, they get stiff and rusty. Gentle, regular motion is what keeps them lubricated and functioning smoothly.
This is particularly true for Osteoarthritis (OA), the most common type, which affected over 528 million people globally as of 2019. For anyone with OA, exercise isn't just a suggestion; it's a foundational part of managing the condition. Building up the muscles around a joint provides much-needed support, and maintaining a healthy weight takes a huge amount of stress off those joints. The World Health Organization has some excellent resources that dive deeper into these non-pharmaceutical strategies.
Gentle, Joint-Friendly Exercises
The trick is to find activities that make you stronger without aggravating the pain. High-impact exercises that involve a lot of pounding, like running on pavement, are often counterproductive. The focus should always be on low-impact movement.
Here are a few options that I often recommend to my patients because they keep the joints moving without the jarring force:
- Swimming and Water Aerobics: Water is your best friend here. Its natural buoyancy supports your body, taking almost all the pressure off your knees, hips, and spine. It’s a fantastic way to build strength and flexibility without the strain.
- Cycling: A stationary bike is a perfect, controlled environment for this. Cycling provides a smooth, repetitive motion that strengthens the major leg muscles that support your knee joints. If you prefer the outdoors, stick to flat, even paths.
- Walking: Don’t underestimate the power of a simple walk. It gets the blood flowing, eases stiffness, and is a great mood-booster. The key is to invest in a good pair of supportive, well-cushioned shoes to absorb the impact.
Don't Forget Strength and Flexibility
Beyond getting your heart rate up, a balanced routine needs to include both strength and flexibility work. These two elements are absolutely crucial for managing arthritis pain.
Strength training isn't about becoming a bodybuilder. It's about building up the muscles that act as shock absorbers for your joints. The stronger those surrounding muscles are, the less stress the joint itself has to endure. You can get great results with resistance bands or simple bodyweight exercises.
A Practical Tip: Always prioritize slow, controlled movements. When you're doing a seated leg lift, for instance, don't just kick your leg out. Instead, consciously tighten your thigh muscle and lift your leg in a smooth, deliberate motion. The quality of the movement matters more than the quantity.
Finally, flexibility is the other side of the coin. Practices like yoga and tai chi are phenomenal for this. They use gentle, flowing movements and stretching to help maintain and even improve your range of motion, which is often the first thing arthritis tries to take away. Tai chi is especially beneficial because it also improves balance, reducing the risk of falls—a serious concern when joints are compromised.
The most important advice I can give is to listen to your body. Start slow, and never push through sharp pain. Learning to adapt your routine on any given day isn't a sign of weakness; it's a sign that you're in tune with your body and managing your health wisely.
Using Nutrition to Fight Inflammation

What you eat has a direct and profound impact on your daily pain levels. Food can either fuel the fire of inflammation, aggravating your joints, or it can be your most powerful tool to calm it down. Shifting toward an anti-inflammatory eating style isn't just a good idea—it's one of the most practical and effective strategies for managing arthritis long-term.
This isn’t about a restrictive, all-or-nothing diet. Think of it as a sustainable lifestyle change, a conscious move toward whole foods packed with compounds that actively fight inflammation where it starts. The goal is to nourish your body, not deprive it.
Building Your Anti-Inflammatory Plate
The core principle here is surprisingly simple: fill your plate with colorful, nutrient-dense foods. I often tell my patients to think of it like painting a vibrant picture at every meal. The more natural colors you see, the more pain-fighting antioxidants and phytonutrients you’re getting.
Here are some of the all-stars you'll want to incorporate right away:
- Fatty Fish: Salmon, mackerel, and sardines are swimming in omega-3 fatty acids, which are famous for their potent anti-inflammatory effects. Try to get at least two servings in per week.
- Colorful Berries: Blueberries, strawberries, and raspberries are loaded with antioxidants that help protect your body from the oxidative stress that can make arthritis symptoms flare.
- Leafy Greens: Spinach, kale, and other dark greens are true nutritional powerhouses. They’re packed with vitamins and minerals that support joint health and can help lower inflammatory markers.
- Nuts and Seeds: Walnuts, flaxseeds, and chia seeds are fantastic plant-based sources of omega-3s. They're perfect for a quick snack or for adding a healthy crunch to salads and oatmeal.
A Quick Tip from Experience: Consistency beats perfection every time. You don't have to overhaul your entire diet overnight. Just start by adding one anti-inflammatory food to each meal—a handful of spinach in your morning omelet, some berries in your yogurt, or a sprinkle of flaxseed on your salad.
Foods That Can Trigger Flare-Ups
Knowing what to add is only half the battle; knowing what to limit is just as crucial. Certain foods are known to promote inflammation, which can make your pain, stiffness, and swelling worse. The usual suspects are almost always found in highly processed items.
It’s a smart move to cut back on:
- Processed Sugars: Think soda, candy, and many packaged snacks. Excess sugar can trigger the release of inflammatory messengers called cytokines.
- Unhealthy Fats: Saturated and trans fats, common in fried foods, fast food, and commercially baked goods, are well-known contributors to systemic inflammation.
Making simple swaps can add up to a huge difference. For instance, trade a sugary breakfast cereal for a warm bowl of oatmeal topped with fresh berries and walnuts. Instead of grabbing a bag of chips, reach for a handful of almonds. Gaining a better understanding of how different foods affect your body is a key step, and for those who want to learn more, there are some great resources explaining how to reduce inflammation through lifestyle.
Finally, managing your nutrition is also directly tied to maintaining a healthy weight. Carrying extra pounds puts a significant amount of mechanical stress on weight-bearing joints like your knees, hips, and back, which can dramatically increase pain. Even a modest weight loss can provide substantial relief, making dietary adjustments a true cornerstone of any effective arthritis management plan.
Navigating Medical and Treatment Options
While lifestyle shifts can make a world of difference, medical treatments are often the bedrock of any solid arthritis management plan. Working closely with your healthcare provider to explore these options is key to getting meaningful relief and, in some cases, actually slowing down the disease's progression. When you know what’s out there, you can have much more effective conversations about your care.
The scale of this issue is immense. In the United States, arthritis impacts nearly 27.9% of adults—that's about 67.1 million people. As a recent CDC report on arthritis prevalence highlights, managing this condition effectively usually means combining medical treatments with the kind of lifestyle adjustments we've been talking about.
Over-The-Counter Pain Relievers
For many people, the first stop for mild to moderate arthritis pain is the local pharmacy aisle. There’s a good reason nonsteroidal anti-inflammatory drugs (NSAIDs) are a popular choice.
Medications like ibuprofen and naproxen work by blocking the chemicals in your body that trigger inflammation. It’s this two-for-one benefit—pain relief plus reduced inflammation—that makes them so helpful for both osteoarthritis and inflammatory arthritis. Even though they’re easy to get, it’s still important to follow the directions and talk to your doctor about long-term use, since they can have side effects.
Prescription Medications for Targeted Relief
When the over-the-counter stuff isn't cutting it, your doctor has a much wider range of tools to work with. These are more powerful treatments, prescribed based on your specific type of arthritis and how severe your symptoms are.
Here are a few common approaches:
-
Corticosteroids: These are potent anti-inflammatories that you can take as a pill or get injected directly into a troublesome joint. A cortisone shot can bring fast, targeted relief during a bad flare-up, calming the fire right where it’s burning.
-
Disease-Modifying Antirheumatic Drugs (DMARDs): If you have an inflammatory condition like rheumatoid arthritis, DMARDs are a game-changer. They don't just mask symptoms; they actually work to quiet the overactive immune system, which can help stop permanent joint damage in its tracks.
-
Biologics: Think of these as a newer, more precise generation of DMARDs. They target very specific parts of the immune system that cause inflammation, offering a highly focused way to manage autoimmune forms of arthritis.
A Note on Holistic Integration: It's important to remember that medical treatments don't operate in a silo. They're most effective when you pair them with supportive therapies. I’ve seen countless patients find an extra layer of relief by combining their medical plan with treatments like acupuncture. It helps manage pain and improve mobility, working in tandem with their prescribed care. You can learn more about how acupuncture for joint pain complements conventional treatments.
At the end of the day, finding the right medical strategy is a partnership between you and your doctor. What works wonders for one person might not be the answer for another. Keeping an open line of communication is the single most important thing you can do to build a plan that truly helps you manage pain and live your life.
Weaving in Mind-Body and Self-Care Practices

Tackling the physical side of arthritis is crucial, but it’s only half the battle. When you're dealing with chronic pain, the mental and emotional strain can be immense. It often creates a vicious cycle: stress and anxiety flare up, which in turn makes the physical pain feel even worse.
This is where integrating mind-body practices and dedicated self-care comes in. These aren't just "nice-to-haves"—they are powerful tools for breaking that pain-stress loop. It’s about learning to calm your nervous system and change your relationship with the pain signals your body is sending. We're looking at the whole person, not just a set of sore joints.
Calming Your Mind to Soothe Your Body
Constant pain puts your nervous system on high alert, stuck in a "fight-or-flight" mode. The goal of mind-body techniques is to consciously shift out of that state and into a place of rest and relaxation, which can have a direct, positive impact on how you perceive pain.
You don’t need to do anything complicated. A few simple practices, done consistently, can make a world of difference.
- Mindfulness Meditation: This practice is about focusing on your breath and simply noticing your thoughts and physical sensations without judging them. The pain might still be there, but meditation helps create a space between you and the sensation, stripping it of its emotional power.
- Deep-Breathing Exercises: When you breathe slowly and deeply from your diaphragm, you're activating the body's natural relaxation response. A simple pattern to try is inhaling for a count of four, holding your breath for four, and then exhaling slowly for a count of six.
The real magic here is quieting the mental chatter that amplifies chronic pain. When you lower your stress hormones, you also help reduce inflammation and the intensity of the pain you feel.
Practical Self-Care You Can Do at Home
Beyond the mental work, some hands-on physical care can provide immediate, tangible relief. These are the simple things you can do every day to manage stiffness and discomfort, especially on those tough flare-up days.
To get started, here are a few simple yet effective techniques you can incorporate into your daily routine.
| Technique | How It Helps | Best For |
|---|---|---|
| Heat Therapy | Increases blood flow, relaxes tight muscles, and soothes stiffness. | Dull, persistent aches and morning stiffness. |
| Cold Therapy | Constricts blood vessels to reduce swelling and numbs the area. | Acute inflammation, sharp pain, or swelling after activity. |
| Gentle Stretching | Improves flexibility and circulation around the joints. | Easing stiffness, especially in the morning or after sitting. |
| Mindful Movement | Activities like Tai Chi or gentle yoga focus on slow, controlled motions. | Improving balance and reducing pain perception. |
These at-home methods give you a sense of control and provide real-time relief when you need it most.
One of the most effective and accessible strategies on that list is temperature therapy. It’s a classic for a reason—it works. By manipulating blood flow and nerve signals, you can directly influence your pain levels.
For example, a warm compress or a long soak in a warm bath is fantastic for easing that deep, chronic stiffness. The heat brings blood to the area, which helps relax everything. On the other hand, an ice pack is your go-to for sharp pain or swelling, like after you’ve overdone it a bit. The cold helps reduce that acute inflammation and provides a welcome numbing effect.
Finally, never underestimate the power of good sleep. We know that poor sleep makes arthritis pain worse. Creating a restful environment is non-negotiable. Make your bedroom as dark and quiet as possible, and stick to a consistent sleep schedule. These foundational habits are a vital part of a holistic strategy for achieving natural chronic pain relief and empowering you to manage your symptoms day in and day out.
Your Questions on Arthritis Pain Answered
Getting an arthritis diagnosis can feel overwhelming, and it often leaves you with a long list of questions. Even when you have a management plan in place, new concerns can crop up from day to day. Having clear, reliable information is key to feeling empowered and in control of your health.
Here, we'll dive into some of the most common questions I hear from patients about managing arthritis pain. My goal is to cut through the noise and give you practical answers you can actually use.
Can Certain Foods Really Make My Arthritis Pain Worse?
Yes, absolutely. For many people, there's a very real connection between what they eat and how their joints feel. Foods that are notorious for kicking up inflammation—things like processed sugars, unhealthy saturated fats, and refined carbs—can make arthritis symptoms feel much worse.
On the other hand, an anti-inflammatory diet can be a game-changer. Think of foods rich in omega-3s (like salmon and walnuts), antioxidants (found in berries and leafy greens), and whole grains. These can actively help dial down your body's inflammatory response. A simple food diary is a great place to start. Just by tracking what you eat and how you feel, you might be surprised to find your own personal trigger foods.
Is It Safe to Exercise When My Joints Are Hurting?
This is a fantastic question, and the answer isn't a simple yes or no. During a severe flare-up, when a joint is red, swollen, and screaming in pain, rest is absolutely what you need. Pushing through that kind of pain can do more harm than good.
However, for that more typical, day-to-day achiness and stiffness, gentle movement is one of the best things you can do. The trick is to choose the right kind of exercise. Low-impact activities are your friend here—things like walking, swimming, or cycling are perfect because they build up the muscles that support your joints without hammering them.
Forget the old "no pain, no gain" motto. That's the worst advice for anyone with arthritis. You have to listen to your body. If an exercise causes sharp or stabbing pain, that’s a clear signal to stop and try something else.
How Is Osteoarthritis Pain Different from Rheumatoid Arthritis Pain?
Understanding this difference is crucial because the treatment approaches are completely different.
Think of osteoarthritis (OA) as a "wear and tear" problem. It's a mechanical issue where the cartilage cushioning your joints breaks down over time. The pain is usually a deep, localized ache that tends to feel worse after activity and gets better with rest.
Rheumatoid arthritis (RA), on the other hand, is an autoimmune condition. This means your own immune system is mistakenly attacking the lining of your joints, causing widespread inflammation. RA pain is often symmetrical (affecting both knees, for example) and usually comes with significant morning stiffness, swelling, and warmth around the joint. Since RA is a systemic disease, treatment has to target the immune system itself, not just the pain.
When Should I See a Doctor for My Joint Pain?
You should never just brush off persistent joint pain as a normal part of getting older. It's always best to get it checked out, especially if the pain is severe or comes with other red flags.
You should definitely make an appointment with your doctor if you're experiencing any of these:
- Significant Swelling: The joint is visibly larger than the one on the other side.
- Redness and Warmth: The skin over the joint looks red or feels warm to the touch.
- Limited Function: The pain is getting in the way of your daily life and activities.
- Prolonged Morning Stiffness: You feel stiff and immobile for more than 30 minutes after you wake up.
Getting an early and accurate diagnosis—especially for an inflammatory condition like RA—is the single most important step you can take to prevent permanent joint damage down the road.
At Eric Tsai Acupuncture and Herbs, we specialize in creating personalized plans that integrate proven traditional methods with modern understanding to help you manage your arthritis pain effectively. Discover how our tailored acupuncture and herbal medicine treatments can help restore your balance and improve your quality of life by visiting us online.