Fibromyalgia presents a complex and deeply personal challenge, characterized by widespread pain, persistent fatigue, and cognitive difficulties that can disrupt daily life. Finding the single "best treatment for fibromyalgia" is often misleading, as a truly effective strategy rarely involves just one approach. Instead, relief is typically found through a customized, multi-faceted plan that addresses the condition's diverse symptoms from several angles. This guide is designed to navigate that complexity, offering a clear and comprehensive roundup of the most effective, evidence-based treatments available today.
We will explore a curated selection of therapeutic options, from pharmacological management and specialized physical therapy to powerful mind-body techniques like Cognitive Behavioral Therapy (CBT) and Mindfulness-Based Stress Reduction (MBSR). Each section provides a structured overview, detailing not only what the treatment involves but also its specific benefits, potential drawbacks, and practical considerations for implementation.
This article moves beyond generic advice to provide actionable insights you can discuss with your healthcare provider. You will learn how to integrate these strategies into a cohesive management plan tailored to your unique symptoms and lifestyle. The goal is to empower you with the knowledge needed to build a sustainable path toward managing pain, improving function, and reclaiming your quality of life.
1. Multimodal Pharmacological Therapy
A cornerstone in managing fibromyalgia is often a carefully tailored pharmacological approach. Rather than relying on a single medication, multimodal therapy involves using a combination of drugs that target different symptoms simultaneously. This strategy recognizes that fibromyalgia is a complex condition with diverse manifestations, including widespread pain, fatigue, sleep disturbances, and cognitive dysfunction (often called "fibro fog").
This combined approach is often considered the best treatment for fibromyalgia from a pharmacological perspective because no single drug effectively addresses all its symptoms. A physician might combine medications that work on different pathways in the central nervous system to achieve a synergistic effect, providing more comprehensive relief than any one drug could alone.
How It Works
Multimodal therapy aims to manage the primary symptoms by targeting their underlying neurological mechanisms. A healthcare provider will select medications from different classes based on a patient's most disruptive symptoms.
- For Pain and Fatigue: Medications originally developed for depression, such as serotonin-norepinephrine reuptake inhibitors (SNRIs), are often prescribed. These drugs, like duloxetine and milnacipran, can modulate pain signals in the brain.
- For Sleep Improvement: Low-dose tricyclic antidepressants, such as amitriptyline, may be used to promote restorative sleep, which is crucial for pain and fatigue management.
- For Neuropathic Pain: Certain anti-seizure medications, including pregabalin and gabapentin, are effective at calming overactive nerve signals that contribute to chronic pain.
Key Insight: The goal of multimodal therapy is not just to mask pain but to re-regulate the central nervous system's pain processing mechanisms, improve sleep quality, and enhance overall function.
A patient experiencing severe pain and insomnia might be prescribed an SNRI for daytime pain relief and a low-dose tricyclic antidepressant at night to improve sleep. By addressing both issues, the patient often experiences a significant improvement in quality of life that would be difficult to achieve with a single medication. This layered strategy allows for lower doses of each drug, potentially reducing the risk of side effects.
2. Graded Exercise Therapy and Low-Impact Aerobics
A foundational element in managing fibromyalgia is a structured and carefully paced exercise regimen. Graded Exercise Therapy (GET) involves a progressive program that gradually increases physical activity, respecting the body's limits to avoid triggering symptom flares. This approach, often combined with low-impact aerobics, is tailored to build cardiovascular fitness, strength, and endurance without over-stressing sensitive muscles and joints.

This method is considered a best treatment for fibromyalgia because it directly counters the deconditioning cycle common in chronic pain. By slowly reintroducing movement, patients can improve physical function, reduce pain perception, and boost mood, making it a powerful non-pharmacological tool for long-term management.
How It Works
Graded Exercise Therapy focuses on establishing a baseline of manageable activity and then incrementally increasing its duration or intensity over time. A physical therapist specializing in chronic pain often designs the program, ensuring it is safe and effective.
- For Cardiovascular Fitness: Activities like walking, swimming, or cycling are started at a very low intensity. For instance, a patient might begin with just five minutes of walking, gradually adding a minute each week.
- For Strength and Flexibility: Gentle strengthening exercises, stretching, and tai chi can improve muscle tone and range of motion. Warm water exercise classes, such as those offered by the Arthritis Foundation, are particularly beneficial as the water's buoyancy supports the body and reduces impact on joints.
- For Consistency: The core principle is consistency over intensity. The goal is to perform some level of activity regularly, preventing the "push-crash" cycle where overexertion leads to days of recovery.
Key Insight: The focus of graded exercise is not on athletic performance but on re-establishing a positive relationship with movement, empowering patients to break the cycle of pain and inactivity safely.
For example, a physical therapist might create a plan starting with 10 minutes of gentle stretching and a 5-minute walk three times a week. The patient would track their symptoms in a journal. If their pain levels remain stable, they might increase the walk to seven minutes the following week. This slow, measured progress helps the central nervous system adapt to activity, reducing pain sensitivity over time.
3. Cognitive Behavioral Therapy (CBT) for Chronic Pain
A powerful psychological approach, Cognitive Behavioral Therapy (CBT) helps individuals manage the mental and emotional toll of fibromyalgia. This structured therapy is not about suggesting the pain is "in your head," but rather it acknowledges the profound connection between the mind and body. It equips patients with skills to change negative thought patterns and behaviors that can amplify pain perception and reduce quality of life.

Many experts consider CBT a best treatment for fibromyalgia because it empowers patients with long-term coping skills. Instead of just treating physical symptoms, it addresses the entire experience of living with chronic pain, helping individuals regain a sense of control over their condition and daily lives. This is a key reason programs like the Mayo Clinic's Pain Rehabilitation Center incorporate CBT so heavily.
How It Works
CBT for chronic pain operates on the principle that thoughts, feelings, and behaviors are interconnected. A therapist specializing in chronic pain helps patients identify and reframe unhelpful thought patterns, such as pain catastrophizing (expecting the worst possible outcome). The focus is on developing practical, actionable coping strategies.
- Identifying Negative Patterns: Patients learn to recognize automatic negative thoughts related to their pain, such as "I can't do anything because of this pain," and challenge their validity.
- Behavioral Pacing: CBT teaches activity pacing, helping individuals find a balance between rest and activity to avoid the boom-and-bust cycle that often worsens symptoms.
- Developing Coping Skills: Techniques include relaxation exercises, stress management, and problem-solving strategies to handle pain flare-ups more effectively.
Key Insight: The goal of CBT is not to eliminate pain but to change one's relationship with it. By modifying thoughts and behaviors, patients can reduce the suffering and disability associated with their physical symptoms.
For example, a patient might use a thought record to track situations that trigger pain flare-ups. They may discover that anticipating a stressful event leads to muscle tension and increased pain. A CBT therapist would help them develop relaxation techniques to use before such events, breaking the cycle and improving their ability to function.
4. Sleep Hygiene and Sleep Disorder Treatment
A critical, yet often overlooked, component in fibromyalgia management is a dedicated focus on sleep. Individuals with fibromyalgia almost universally suffer from non-restorative sleep, where they wake up feeling as tired as when they went to bed. This treatment approach addresses sleep quality through a dual strategy: establishing rigorous sleep hygiene practices and medically treating underlying sleep disorders.
This focus on sleep is often considered one of the best treatments for fibromyalgia because poor sleep directly exacerbates pain, fatigue, and cognitive dysfunction. By improving sleep quality, the body’s natural pain modulation and restorative processes can function more effectively, leading to a significant reduction in core fibromyalgia symptoms.
How It Works
This approach systematically identifies and corrects factors that disrupt sleep. A healthcare provider, often in collaboration with a sleep specialist, will recommend behavioral changes and, if necessary, medical interventions to restore healthy sleep cycles.
- For Sleep Quality: Implementing strict sleep hygiene is the first step. This includes maintaining a consistent sleep-wake schedule, even on weekends, and creating an optimized sleep environment.
- For Underlying Disorders: Many fibromyalgia patients have comorbid sleep disorders like sleep apnea or restless leg syndrome. A formal sleep study (polysomnography) may be recommended to diagnose these conditions so they can be treated directly.
- For Pain and Comfort: Optimizing your sleeping environment is paramount, particularly for managing pain. Investing in the right bedding and mattress support can drastically improve comfort and reduce nocturnal disturbances. For instance, exploring options like this A complete guide to mattress toppers for back pain can help individuals find solutions to alleviate pressure points and minimize sleep disruptions.
Key Insight: The goal is not just to get more hours of sleep, but to increase the amount of deep, restorative sleep, which is essential for muscle repair, memory consolidation, and regulating pain-processing neurotransmitters.
A patient might start by eliminating screen time before bed and ensuring their bedroom is cool, dark, and quiet. If symptoms persist, a sleep study could reveal obstructive sleep apnea, leading to treatment with a CPAP machine. This combination of behavioral adjustments and medical treatment can dramatically improve energy levels and decrease pain sensitivity.
5. Mindfulness-Based Stress Reduction (MBSR) and Meditation
Mind-body therapies like Mindfulness-Based Stress Reduction (MBSR) offer a powerful, non-pharmacological approach to managing fibromyalgia. This structured, 8-week program teaches participants to cultivate moment-to-moment awareness of their thoughts, feelings, and bodily sensations without judgment. This practice helps individuals change their relationship with pain, reducing the distress and emotional reactivity often associated with chronic conditions.
For many, MBSR is considered the best treatment for fibromyalgia from a self-management perspective because it empowers patients with tools to regulate their own nervous system. Instead of being controlled by pain signals, individuals learn to observe them, which can lessen their intensity and impact on daily life.
How It Works
MBSR systematically trains the brain to reduce stress reactivity and improve emotional regulation through formal and informal mindfulness practices. The program, originally developed by Dr. Jon Kabat-Zinn, combines meditation, body awareness, and gentle mindful movement to address the core symptoms of fibromyalgia.
- For Pain Perception: Mindfulness meditation helps break the cycle of pain, stress, and anxiety. By focusing on the present, patients can detach from catastrophic thinking about their pain, which can decrease its perceived severity.
- For Stress and Anxiety: Through techniques like the body scan and sitting meditation, participants learn to recognize stress triggers and calm the body's physiological stress response. You can learn more about how to reduce anxiety naturally through these methods.
- For Cognitive Function: Regular mindfulness practice has been shown to improve focus and reduce "fibro fog" by strengthening the brain's attention networks.
Key Insight: The objective of MBSR is not to eliminate pain but to fundamentally change your relationship with it. It teaches you to live well despite pain by reducing the suffering that often accompanies it.
A typical approach involves starting with short, guided meditations, perhaps just five minutes a day, using an app or online program. Gradually, you can increase the duration as you build consistency. For instance, reputable programs like those offered at the University of Massachusetts or Duke Integrative Medicine provide a structured curriculum that has been specifically adapted for chronic pain management.
6. Nutritional and Anti-Inflammatory Diet Interventions
A growing body of evidence suggests that dietary choices play a significant role in managing fibromyalgia symptoms. This approach focuses on reducing systemic inflammation, addressing common nutritional deficiencies, and identifying potential food triggers that can worsen pain and fatigue. For many, a targeted nutritional strategy is a foundational component of the best treatment for fibromyalgia, as it empowers patients to take control of their health through daily habits.

This method moves beyond generic "healthy eating" advice and delves into the biochemical impact of food on chronic pain pathways. By adopting an anti-inflammatory diet rich in whole foods and eliminating processed ingredients and potential irritants, individuals can create an internal environment that supports pain reduction and improved energy levels.
How It Works
Nutritional interventions aim to calm an overactive immune system and provide the body with the micronutrients needed to function optimally. A registered dietitian or a functional medicine practitioner can guide patients through a personalized plan based on their unique symptoms and potential sensitivities.
- Anti-Inflammatory Focus: This involves increasing the intake of foods high in omega-3 fatty acids, antioxidants, and phytonutrients, such as fatty fish, leafy greens, and colorful vegetables. When considering specific foods that support an anti-inflammatory diet, exploring the nutritional benefits of various fruits can be highly beneficial; this simple guide to mixed berries nutrition facts offers a great example.
- Elimination Protocols: Some individuals find relief by temporarily removing common inflammatory triggers like gluten, dairy, and artificial additives. A food and symptom diary is crucial for identifying which foods may be linked to symptom flare-ups.
- Targeted Supplementation: Many people with fibromyalgia have deficiencies in key nutrients like vitamin D, magnesium, and B vitamins. A healthcare provider can order blood tests to identify these deficiencies and recommend appropriate supplements to support nerve function and energy production. Learn more about how to reduce inflammation through targeted strategies.
Key Insight: The goal of nutritional intervention is to reduce the body's overall inflammatory load, which can directly impact the central nervous system's sensitivity to pain and help alleviate widespread fibromyalgia symptoms.
A practical approach might involve starting with small, sustainable changes, such as replacing processed snacks with whole fruits and nuts, and then gradually progressing to a more structured plan. Working with a professional, such as those at the Cleveland Clinic's functional medicine programs, ensures the approach is safe, effective, and tailored to individual needs.
7. Integrative Manual Therapies
Integrative manual therapies offer a hands-on approach to fibromyalgia management, combining several therapeutic techniques to address the condition's musculoskeletal symptoms. This approach includes methods like massage therapy, myofascial release, trigger point therapy, and gentle chiropractic care, all specifically adapted for the unique sensitivities of fibromyalgia patients. It focuses on reducing muscle tension, improving local circulation, and promoting nervous system relaxation.
This multifaceted hands-on strategy is often considered a supportive candidate for the best treatment for fibromyalgia for those seeking non-pharmacological relief. It acknowledges that physical discomfort and central nervous system sensitivity are deeply connected. A skilled practitioner can provide targeted relief to painful areas while using gentle techniques that do not overstimulate the system, which is a common risk with more aggressive bodywork.
How It Works
Integrative manual therapies work by directly addressing the soft tissues and joints, aiming to alleviate the chronic pain and stiffness characteristic of fibromyalgia. A therapist will customize the session based on a patient's specific pain points and tolerance levels, a crucial step for avoiding post-treatment flare-ups.
- For Muscle Tension and Tender Points: Techniques like gentle massage and trigger point therapy apply careful pressure to release knots and reduce localized pain in hyper-irritable spots.
- For Widespread Stiffness: Myofascial release involves applying sustained, gentle pressure to stretch the connective tissue (fascia) that envelops muscles, helping to restore mobility and reduce a sense of full-body restriction.
- For Structural Alignment and Nerve Function: Gentle chiropractic adjustments can help improve spinal alignment, which may reduce nerve irritation and enhance overall physical function.
Key Insight: The primary goal of integrative manual therapies is to calm the overactive nervous system through therapeutic touch, breaking the cycle of pain and muscle tension without causing the systemic stress that can trigger a flare.
For instance, a patient with severe shoulder and neck tension might benefit from a session that combines gentle myofascial release to address fascial restrictions with targeted trigger point therapy on specific knots. Starting with shorter sessions and communicating clearly with a therapist who has experience with fibromyalgia is essential for success. This approach allows the body to adapt and helps build a foundation for long-term pain management.
8. Comprehensive Pain Management Programs
For individuals whose fibromyalgia symptoms are severe, persistent, and disruptive to daily life, a comprehensive pain management program offers an intensive, structured approach. These multidisciplinary programs integrate medical, psychological, and physical therapies into a single, coordinated treatment plan. This immersive strategy addresses the whole person, not just isolated symptoms, acknowledging the interconnected nature of chronic pain, mental health, and physical function.
This integrated model is often considered the best treatment for fibromyalgia for those who have not found relief with single-modality treatments. By bringing a team of specialists together, these programs provide a level of care and collaboration that is difficult to replicate through separate appointments with different providers. The goal is to empower patients with skills and strategies to manage their condition long-term.
How It Works
Comprehensive pain management programs are typically intensive, often requiring daily participation for several weeks. A team of experts, including physicians, psychologists, and physical therapists, collaborates to create a personalized plan that addresses the patient's specific needs and goals.
- Medical Management: Physicians oversee medication adjustments and manage any co-occurring medical conditions.
- Physical and Occupational Therapy: Therapists design tailored exercise regimens to improve strength, flexibility, and function while teaching pacing strategies to avoid flare-ups.
- Psychological Support: Psychologists provide counseling, often using Cognitive Behavioral Therapy (CBT), to help patients reframe negative thought patterns about pain and develop effective coping mechanisms.
For a quick reference, here is a summary of what these intensive programs typically entail.
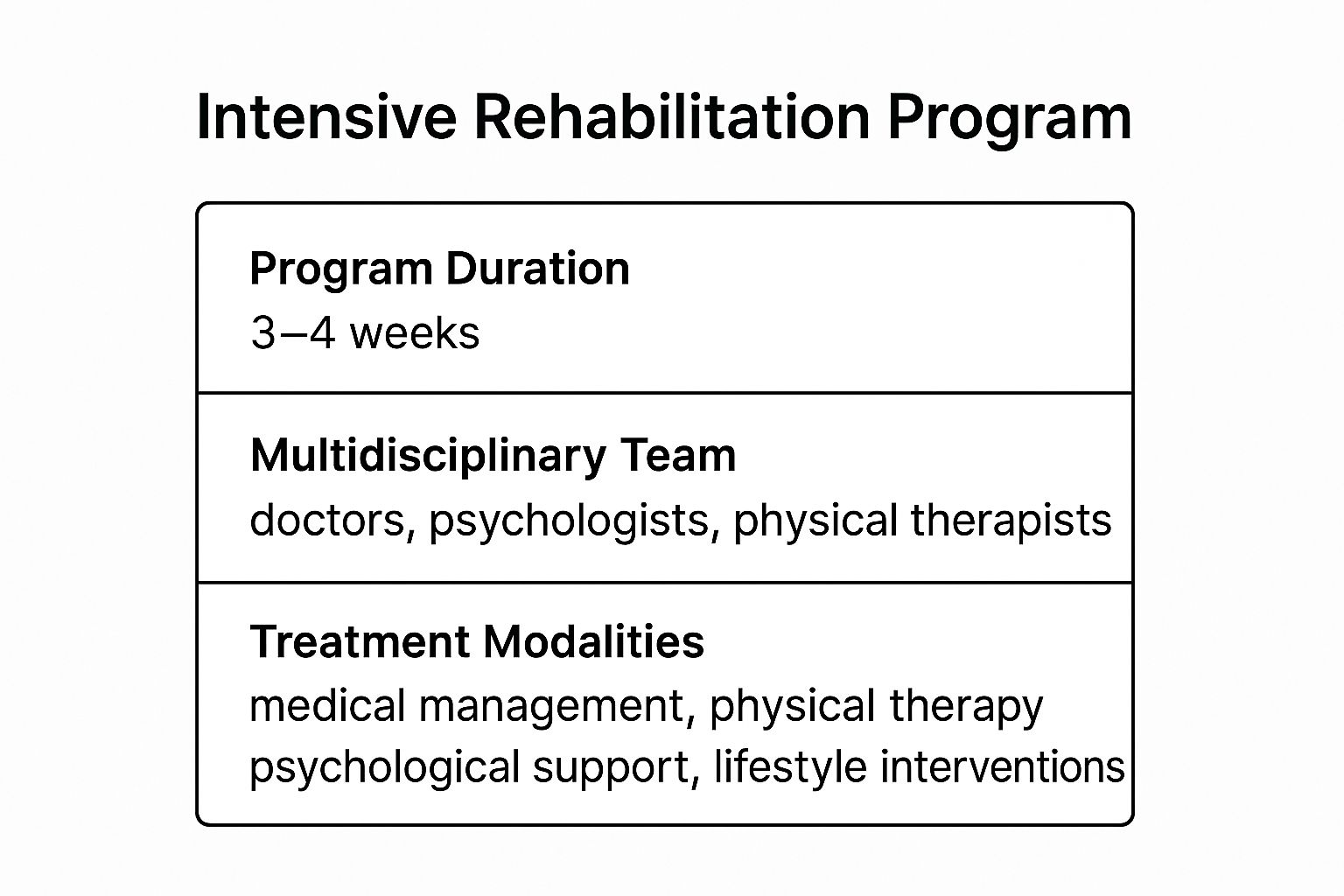
This visual highlights the core components, showing how a dedicated team uses multiple modalities over a concentrated period to achieve results.
Key Insight: The primary objective of these programs is functional restoration. The focus shifts from curing pain to improving quality of life and empowering patients to manage their symptoms independently.
For instance, a patient might learn stress-reduction techniques from a psychologist in the morning, participate in a gentle aquatic therapy session with a physical therapist mid-day, and attend an educational seminar on sleep hygiene in the afternoon. This holistic, all-in-one approach ensures that all facets of fibromyalgia are addressed simultaneously, leading to more sustainable improvements in function and well-being. Prominent examples include programs at the Mayo Clinic Pain Rehabilitation Center and the Cleveland Clinic.
Top 8 Fibromyalgia Treatment Comparison
| Treatment Approach | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Multimodal Pharmacological Therapy | Moderate to high 🔄🔄 | Requires medications, specialist visits ⚡⚡ | Moderate to high pain reduction (30-50%) 📊 | Patients needing multi-symptom pharmaceutical management 💡 | Evidence-based, targets multiple pathways ⭐⭐ |
| Graded Exercise Therapy & Low-Impact Aerobics | Moderate 🔄 | Time commitment, possible physical therapy ⚡ | Improved fitness, reduced stiffness & pain 📊 | Patients able to engage in structured physical activity 💡 | No medication side effects, cost-effective ⭐ |
| Cognitive Behavioral Therapy (CBT) | Moderate to high 🔄🔄 | Requires specialized therapists, time ⚡ | Long-lasting coping skills, mental health gains 📊 | Patients with chronic pain-related emotional distress 💡 | Addresses mental & physical pain, no side effects ⭐ |
| Sleep Hygiene & Sleep Disorder Treatment | Moderate 🔄 | Sleep studies, lifestyle adjustments ⚡ | Improved sleep quality, energy, reduced pain 📊 | Patients with fibromyalgia-related sleep disturbances 💡 | Addresses root causes, enhances other treatments ⭐ |
| Mindfulness-Based Stress Reduction (MBSR) | Moderate 🔄 | Weekly sessions plus daily practice ⚡ | Reduced pain intensity & emotional distress 📊 | Patients interested in non-pharmacologic stress reduction 💡 | Lifelong skills, no side effects ⭐ |
| Nutritional and Anti-Inflammatory Diet | Low to moderate 🔄 | Dietary changes, possible supplements ⚡ | Reduced inflammation, improved energy 📊 | Patients with inflammation and dietary sensitivities 💡 | Low risk, overall health benefits ⭐ |
| Integrative Manual Therapies | Low to moderate 🔄 | Skilled therapists, frequent sessions ⚡ | Immediate symptom relief, muscle relaxation 📊 | Patients seeking non-pharmaceutical symptom relief 💡 | Promotes relaxation, reduces muscle tension ⭐ |
| Comprehensive Pain Management Programs | High 🔄🔄🔄 | Multidisciplinary team, intensive program ⚡⚡⚡ | Significant overall improvement 📊 | Patients needing intensive, coordinated care 💡 | Addresses all fibromyalgia aspects, strong evidence base ⭐⭐ |
Crafting Your Personalized Fibromyalgia Treatment Plan
Navigating the landscape of fibromyalgia treatments can often feel overwhelming, but as we've explored, a wealth of effective options exists. The journey from diagnosis to relief is not about finding a single "magic bullet." Instead, the key takeaway is that the best treatment for fibromyalgia is a personalized, multi-faceted strategy that addresses your unique symptoms, lifestyle, and wellness goals. We've examined a range of powerful interventions, from multimodal medications and graded exercise to cognitive behavioral therapy and nutritional changes, each offering a distinct pathway to reclaiming control over your health.
The true power lies in synergy. A pharmacological approach might lower the baseline pain enough to make physical therapy effective. Simultaneously, mindfulness-based stress reduction can help you manage the emotional toll of flare-ups, while improved sleep hygiene restores your body’s ability to heal. No single intervention works in isolation; they are interconnected components of a comprehensive wellness architecture.
Your Actionable Next Steps to Relief
Moving forward from information to implementation is the most critical step. Rather than trying to adopt every strategy at once, focus on a methodical, sustainable approach.
- Start with a Comprehensive Assessment: Your first action should be a detailed discussion with a healthcare provider who understands the complexities of fibromyalgia. Bring this list of treatments to your appointment to facilitate a collaborative conversation about where to begin.
- Identify Your Biggest Hurdle: What symptom impacts your quality of life the most? Is it debilitating fatigue, persistent pain, or overwhelming brain fog? Prioritize a treatment that directly targets this primary challenge. For instance, if sleep is your main issue, focusing on sleep hygiene and consulting a sleep specialist may provide the most immediate and significant benefits.
- Build a Multidisciplinary Team: Fibromyalgia is a complex condition that often requires a team approach. This team might include your primary care physician, a rheumatologist, a physical therapist, a mental health professional, and a specialist in complementary medicine like an acupuncturist. Each professional brings a unique and valuable perspective to your care.
- Track Your Progress Diligently: Use a journal or a health tracking app to monitor your symptoms, energy levels, pain scores, and mood. This data is invaluable for you and your healthcare team to objectively assess what’s working and what needs adjustment. This patient-led evidence is crucial for refining your long-term management plan.
Mastering these approaches means shifting your mindset from passively seeking a cure to actively constructing a personalized system for managing your condition. This proactive stance is empowering and is often the turning point for individuals living with fibromyalgia. By integrating these strategies, you are not just treating symptoms; you are building a resilient foundation for long-term well-being, improved function, and a higher quality of life. The path to managing fibromyalgia is a marathon, not a sprint, and your commitment to this personalized, integrated approach is your most powerful tool.
If you are seeking a holistic, evidence-based approach to complement your fibromyalgia management plan, consider the benefits of traditional Chinese medicine. At Eric Tsai Acupuncture and Herbs, we specialize in creating personalized treatment protocols that integrate acupuncture and herbal medicine to reduce pain, manage stress, and restore balance. Visit us at Eric Tsai Acupuncture and Herbs to learn how we can support your journey toward lasting relief.