Irritable Bowel Syndrome (IBS) is more than just an occasional inconvenience; it's a chronic condition that can profoundly impact daily life with its unpredictable cycle of bloating, gas, abdominal pain, and fluctuating bowel habits. For the millions affected, finding a consistent path to relief can feel overwhelming. While there is no universal cure for IBS, a growing body of evidence highlights a range of powerful strategies that can effectively manage symptoms and restore digestive harmony. This guide is designed to cut through the noise and offer a comprehensive look at some of the best remedies for IBS, moving past generic advice to deliver practical, actionable solutions.
This article provides a detailed roundup of the most effective, science-backed approaches available. We will explore powerful interventions, including targeted dietary protocols like the Low FODMAP diet, specific natural supplements such as peppermint oil and psyllium husk, and transformative mind-body therapies that directly address the sensitive gut-brain connection. The focus here is on empowering you with a personalized toolkit of strategies, complete with specific implementation details and what to expect from each. By understanding how these remedies work, you can begin to build a customized management plan to regain control over your symptoms and significantly improve your overall quality of life. We will delve into multi-strain probiotics, the role of regular physical exercise, and even the innovative approach of gut-directed hypnotherapy, giving you a clear roadmap to lasting relief.
1. Low FODMAP Diet
For many individuals navigating the complexities of Irritable Bowel Syndrome (IBS), the Low FODMAP Diet stands out as one of the most effective and scientifically validated remedies available. Developed by researchers at Monash University, this dietary approach is a powerful tool for identifying specific food triggers that cause symptoms like bloating, gas, abdominal pain, diarrhea, and constipation.
What Are FODMAPs?
FODMAP is an acronym for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are short-chain carbohydrates that are poorly absorbed in the small intestine. When they reach the large intestine, they are rapidly fermented by gut bacteria, drawing in water and producing gas. This process can lead to significant discomfort and digestive distress in people with IBS.
The diet is not a lifelong restriction but a structured, multi-phase process designed to pinpoint personal triggers. Research from Monash University found that up to 76% of individuals with IBS experienced significant symptom improvement after following the protocol. Its efficacy is so well-regarded that it is now recommended as a first-line dietary treatment by health organizations like the UK's National Health Service (NHS).
The Three-Phase Protocol
The Low FODMAP Diet is a systematic journey, not a simple list of "good" and "bad" foods. The following infographic illustrates the structured, three-phase process essential for success.
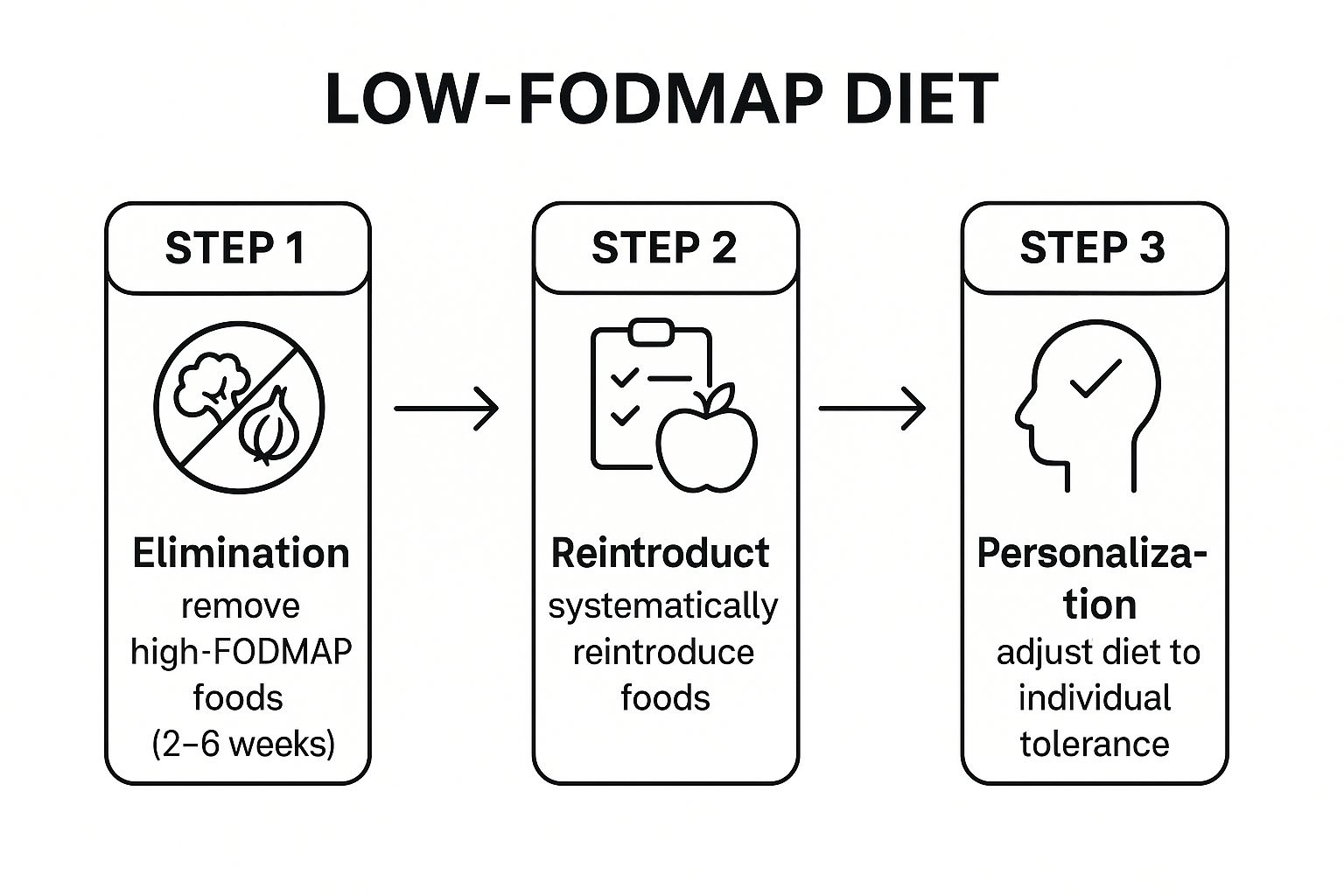
This step-by-step approach ensures that dietary restrictions are temporary and that the final diet is as varied and nutritionally complete as possible.
How to Implement the Low FODMAP Diet
Successfully navigating this diet requires guidance and precision. Skipping steps or reintroducing foods randomly can lead to inaccurate results and unnecessary long-term restrictions.
- Work with a Professional: Collaborate with a registered dietitian specializing in the FODMAP protocol. They can ensure you maintain nutritional balance during the elimination phase and guide you through reintroduction correctly.
- Use Reliable Resources: The Monash University FODMAP Diet App is the gold standard for identifying high and low FODMAP foods, with up-to-date information and portion size guidance.
- Keep a Detailed Diary: Track your food intake, portion sizes, and any corresponding symptoms. This log is crucial for identifying patterns during the reintroduction phase.
- Embrace the Reintroduction Phase: The ultimate goal is to expand your diet, not restrict it. Systematically reintroducing food groups helps you understand your personal tolerance levels, leading to a sustainable, long-term eating plan.
The Low FODMAP diet is one of the best remedies for IBS because it empowers you with knowledge about your own body, transforming a confusing condition into a manageable one. For more information on creating a gut-friendly eating plan, discover more about the best foods for digestive health.
2. Peppermint Oil Supplements
For individuals seeking a natural remedy to calm the painful spasms associated with Irritable Bowel Syndrome (IBS), peppermint oil supplements offer a potent and well-researched solution. This traditional remedy has gained significant validation from modern science, positioning it as a first-line treatment for managing abdominal pain, cramping, and bloating in many clinical guidelines.
How Does Peppermint Oil Work?
The primary active compound in peppermint oil is L-menthol. This compound has a direct antispasmodic effect on the smooth muscles of the digestive tract. When delivered directly to the intestines, L-menthol blocks calcium channels in muscle cells, which helps them relax and reduces the intensity and frequency of painful contractions that are common in IBS.
To be effective and avoid common side effects like heartburn, the supplements must be enteric-coated. This special coating ensures the capsule bypasses the stomach acid and dissolves only when it reaches the small intestine, delivering the soothing properties of peppermint oil exactly where they are needed most. The efficacy of this approach is well-documented; a meta-analysis of 12 clinical trials published in BMC Complementary and Alternative Medicine confirmed that peppermint oil significantly improves IBS symptoms, particularly abdominal pain.
Targeted Relief with Proven Results
The scientific community, including gastroenterology researcher Dr. Alex Ford, has extensively studied peppermint oil's role in IBS management. Its targeted mechanism is why it is often recommended as one of the best remedies for IBS.
Commercial products like IBgard have demonstrated this effectiveness in clinical settings. In one study, patients taking IBgard reported a 40% reduction in their total IBS symptom score compared to a placebo. This level of evidence has led to its recommendation by organizations such as the American College of Gastroenterology for providing global symptom relief.
How to Use Peppermint Oil Supplements
To maximize benefits and minimize potential side effects, it's crucial to use peppermint oil supplements correctly. Improper use can lead to heartburn or reduce the supplement's effectiveness.
- Choose Enteric-Coated Formulas: This is non-negotiable. Only enteric-coated capsules can deliver the oil to the intestines without causing irritation in the stomach or esophagus.
- Time Your Doses: For best results, take one capsule 30 to 60 minutes before meals on an empty stomach. This allows the oil to reach the intestines and begin its work before food arrives, preventing food-triggered spasms.
- Start with a Low Dose: Begin with the lowest recommended dose on the product label to assess your tolerance. You can gradually increase it if needed, following the package instructions or a doctor's advice.
- Avoid Taking with Antacids: Antacids reduce stomach acid, which can cause the enteric coating to dissolve prematurely in the stomach. This can lead to heartburn and negates the targeted delivery mechanism.
When used correctly, peppermint oil provides a safe and effective way to manage the core symptoms of IBS, offering a natural path to significant relief and improved quality of life. For a deeper look into dietary strategies that complement these remedies, you can learn more about our approach to digestive wellness.
3. Probiotics (Multi-strain formulations)
Among the most promising and well-researched remedies for IBS, targeted probiotic therapy offers a way to directly address gut microbiome imbalances often implicated in symptoms. Probiotics are live beneficial bacteria that, when consumed in adequate amounts, can help restore microbial harmony, reduce gut inflammation, and improve intestinal barrier function. For those with IBS, multi-strain formulations are often more effective as they provide a diverse range of bacterial species to address the complex ecosystem of the gut.
What Are Multi-Strain Probiotics?
Multi-strain probiotics are supplements containing several different species and strains of beneficial bacteria, such as various types of Lactobacillus and Bifidobacterium. The rationale is that a combination of strains can perform a wider array of functions than a single strain alone, more closely mimicking the natural diversity of a healthy gut microbiome. This synergistic approach can be more effective at alleviating a broad spectrum of IBS symptoms, from bloating and gas to irregular bowel movements.
The efficacy of specific probiotic formulations in managing IBS is supported by significant clinical evidence. For instance, the high-potency, multi-strain probiotic VSL#3 has demonstrated effectiveness in reducing bloating and pain in patients with IBS-D. Similarly, Symprove, a water-based liquid probiotic, showed significant symptom improvement in a large independent clinical trial. Even single-strain products like Align (Bifidobacterium 35624) have shown such success that they paved the way for more complex multi-strain developments.
How to Implement Probiotic Therapy
Successfully using probiotics for IBS requires a strategic and patient approach. Simply grabbing any bottle off the shelf is unlikely to yield results; the key is choosing a quality product and using it correctly.
- Choose Clinically Studied Strains: Look for products containing strains that have been researched for IBS, such as Bifidobacterium infantis 35624, Lactobacillus plantarum 299v, or combinations found in products like VSL#3 or Symprove.
- Start Low and Go Slow: Begin with a lower dose than recommended on the package and gradually increase over one to two weeks. This allows your gut to adjust and minimizes the risk of temporary side effects like gas or bloating.
- Be Consistent and Patient: Take your probiotic daily for at least 4-8 weeks before evaluating its effectiveness. It takes time for the beneficial bacteria to colonize the gut and exert their effects.
- Ensure Viability and Potency: Opt for reputable brands that provide third-party testing and guarantee potency through the expiration date. Some formulations may require refrigeration to maintain the viability of the live cultures.
Probiotics are one of the best remedies for IBS because they target a root cause: dysbiosis. By rebalancing the gut microbiota, they offer a foundational approach to long-term symptom management. For a deeper look into other natural gut-soothing options, you can explore more about herbal remedies for IBS.
4. Psyllium Husk Fiber Supplementation
For individuals struggling with the unpredictable nature of Irritable Bowel Syndrome (IBS), psyllium husk fiber emerges as a remarkably versatile and effective remedy. This soluble fiber, derived from the seeds of the Plantago ovata plant, acts as a bulk-forming agent that can uniquely normalize bowel function for both constipation-predominant (IBS-C) and diarrhea-predominant (IBS-D) subtypes, making it one of the best remedies for IBS management.
How Does Psyllium Work?
Psyllium’s power lies in its ability to absorb and hold water. When mixed with liquid, it forms a viscous, gel-like substance. In cases of IBS-C, this gel softens stool and adds bulk, making it easier to pass and promoting regularity. Conversely, for those with IBS-D, the gel absorbs excess fluid in the colon, which helps to form more solid stools and reduce the frequency and urgency of bowel movements.
This dual-action capability is supported by significant research. Clinical studies, including those analyzing products like Metamucil, have repeatedly demonstrated psyllium's ability to improve overall IBS symptoms, including abdominal pain and bloating. Its efficacy is so well-established that the American Gastroenterological Association (AGA) recommends soluble fiber like psyllium as a primary treatment option for global IBS symptoms.
Why Psyllium Over Other Fibers?
Not all fibers are created equal, especially for a sensitive gut. While insoluble fibers like wheat bran can sometimes aggravate IBS symptoms by increasing gas and bloating, psyllium is generally better tolerated. Its slow fermentation rate means it produces less gas in the gut compared to other fibers, offering relief without the common side effect of increased discomfort. This makes it a superior choice for many seeking symptom control.
How to Implement Psyllium Husk Supplementation
Introducing psyllium correctly is key to harnessing its benefits without causing digestive upset. A "low and slow" approach prevents the body from being overwhelmed.
- Start with a Small Dose: Begin with one teaspoon (approximately 3-5 grams) mixed into a full glass of liquid once a day. Gradually increase the dose over several days or weeks to find what works for you, typically aiming for 1-2 tablespoons daily.
- Hydration is Crucial: Always mix psyllium with at least 8 ounces (240 ml) of water or another liquid and drink it immediately before it thickens. It is also essential to increase your overall water intake throughout the day to help the fiber work effectively and prevent blockages.
- Time it Right: To avoid interfering with the absorption of other substances, take medications or other supplements at least one hour before or four hours after consuming psyllium.
- Listen to Your Body: Pay close attention to how your body responds. If you experience increased gas or bloating, reduce the dose and increase it more slowly. The goal is gentle, consistent regulation, not a sudden shock to your system.
5. Stress Management and Cognitive Behavioral Therapy (CBT)
The powerful connection between the gut and the brain is central to the experience of Irritable Bowel Syndrome (IBS). For this reason, addressing psychological factors is one of the best remedies for IBS, offering profound relief where other treatments may fall short. Stress management techniques, particularly Cognitive Behavioral Therapy (CBT), provide a structured, evidence-based approach to calming this gut-brain axis and reducing symptom severity.
What Is Gut-Directed CBT?
Cognitive Behavioral Therapy (CBT) is a type of psychotherapy that helps individuals identify and change destructive or unhelpful thinking patterns and behaviors. Gut-directed CBT specifically applies these principles to the cycle of anxiety, stress, and physical symptoms common in IBS. It teaches you to reframe your thoughts about pain and discomfort, develop effective coping mechanisms, and break the feedback loop where stress triggers gut symptoms, which in turn causes more stress.
The effectiveness of this approach is well-documented. A pioneering web-based CBT program from Manchester University demonstrated that 70% of participants experienced significant symptom improvement. Similarly, research from institutions like UCLA on Mindfulness-Based Stress Reduction highlights how mind-body therapies can directly influence gut function and perception of pain.
Targeting the Root of the Gut-Brain Dysfunction
Unlike remedies that only target digestive processes, CBT addresses the neurological and psychological drivers of IBS. It helps patients manage the hypervigilance and catastrophic thinking that often accompany chronic digestive issues, such as the constant fear of a flare-up in public. Given the strong link between anxiety and IBS symptoms, understanding specific ways therapy can help manage anxiety is a vital step towards finding relief. By learning to control the stress response, you can directly reduce the visceral hypersensitivity that makes the gut overreact to normal stimuli.
How to Implement CBT and Stress Management
Integrating these powerful techniques into your IBS management plan requires a proactive and consistent approach. The goal is to build resilience so that life's daily stressors no longer translate into digestive distress.
- Seek Specialized Support: Look for a therapist trained in gut-directed CBT or health psychology. Pioneers like Dr. Jeffrey Lackner and Dr. Olafur Palsson have developed specific protocols that are highly effective for IBS.
- Keep a Stress-Symptom Diary: Just as you would for food, track your stress levels, emotional state, and corresponding gut symptoms. This helps you and your therapist identify specific psychological triggers.
- Practice Consistently: Incorporate relaxation techniques like deep breathing, meditation, or progressive muscle relaxation into your daily routine. Consistency is key to retraining your nervous system's response.
- Explore Digital Tools: Consider evidence-based apps designed for IBS, such as Zemedy or Mahana IBS, which offer structured CBT programs you can follow from home.
By addressing the "brain" part of the gut-brain axis, CBT and stress management offer a transformative path to lasting symptom control. For more actionable strategies on managing daily pressures, learn how to cope with stress effectively.
6. Regular Physical Exercise
Beyond its well-known benefits for cardiovascular health and mood, regular physical exercise has emerged as a powerful, non-pharmacological remedy for managing Irritable Bowel Syndrome (IBS). It works by addressing both the physical and psychological components of the condition, helping to regulate gut motility, reduce stress, and improve the intricate communication along the gut-brain axis.

How Exercise Influences IBS Symptoms
Physical activity directly impacts several mechanisms that contribute to IBS flare-ups. Gentle, consistent movement helps stimulate normal bowel contractions, which can alleviate constipation and reduce feelings of bloating. Simultaneously, exercise is a proven stress-reducer, lowering levels of cortisol, a hormone that can exacerbate gut sensitivity and discomfort.
The efficacy of this approach is backed by significant research. A notable Swedish study led by Dr. Riadh Sadik at the University of Gothenburg found that patients with IBS who engaged in moderate physical activity for 20-60 minutes, three to five times per week, experienced a 43% reduction in symptom severity. This highlights why structured movement is considered one of the best remedies for IBS, offering a way to actively manage the condition.
Which Types of Exercise Are Best?
The ideal exercise for IBS is one that you can perform consistently without triggering symptoms. High-intensity workouts can sometimes worsen symptoms like cramping or diarrhea in sensitive individuals, so finding the right balance is key.
Integrative gastroenterology programs often recommend a combination of low-to-moderate intensity activities. Yoga, for example, combines gentle physical postures with breathing exercises and mindfulness, which helps calm the nervous system and reduce visceral hypersensitivity. Similarly, Tai Chi offers a low-impact way to improve both physical and mental well-being.
How to Implement an IBS-Friendly Exercise Routine
Starting a new exercise regimen should be a gradual and mindful process. The goal is to build a sustainable habit that soothes your digestive system, not shocks it.
- Start Slowly and Gently: If you are new to exercise, begin with 15-20 minutes of low-impact activity, such as walking or cycling, three times a week. Gradually increase the duration and frequency as your body adapts.
- Prioritize Consistency: Regular, moderate activity is more beneficial for regulating gut function than occasional, intense workouts. Aim for consistency over intensity.
- Listen to Your Body: Pay close attention to how different activities affect your symptoms. If high-impact exercises like running cause flare-ups, switch to gentler options like swimming or using an elliptical machine.
- Incorporate Mind-Body Practices: Consider adding yoga or tai chi to your routine. These practices are uniquely suited for IBS as they directly address the stress component via the gut-brain axis, enhancing both physical and emotional resilience.
Regular physical exercise empowers you to take an active role in your health, offering a sustainable and effective strategy for long-term symptom management. For a holistic approach that integrates lifestyle changes with targeted treatments, learn more about our personalized wellness plans.
7. Gut-Directed Hypnotherapy
Among the most innovative and effective remedies for IBS is Gut-Directed Hypnotherapy (GDH), a specialized mind-body therapy that harnesses the powerful connection between the brain and the digestive system. This clinical approach uses guided relaxation, focused attention, and therapeutic suggestions to influence gut function, reduce pain sensitivity, and restore normal intestinal motility. It directly addresses the visceral hypersensitivity and dysregulation that are hallmarks of IBS.
What is Gut-Directed Hypnotherapy?
Gut-Directed Hypnotherapy is a form of clinical hypnosis specifically tailored to address gastrointestinal disorders. During a session, a trained therapist guides the individual into a state of deep relaxation and focused awareness. In this state, the therapist provides suggestions aimed at calming and normalizing the gut. These suggestions might include visualizing a smooth, comfortable digestive process or imagining reduced sensitivity in the intestinal nerves.
The efficacy of GDH is supported by significant scientific evidence. Pioneering research from Professor Peter Whorwell at the University of Manchester found that approximately 71% of patients experienced significant and lasting improvement in their IBS symptoms after undergoing the therapy. Further studies, including clinical trials at Monash University, have reaffirmed its benefits, showing that improvements can persist for years after the initial treatment course concludes.
The Gut-Brain Axis in Action
GDH is not a psychological placebo; it is a targeted intervention that directly influences the gut-brain axis, the complex communication network linking your central nervous system with your enteric nervous system (the "second brain" in your gut). The therapy works by retraining the brain's perception of and response to signals from the gut, effectively turning down the "volume" on pain and discomfort signals.
This makes it one of the best remedies for IBS, particularly for individuals who have not responded well to dietary or pharmacological treatments. Its ability to modify the root neurological pathways of IBS symptoms provides a unique and powerful pathway to relief.
How to Implement Gut-Directed Hypnotherapy
To explore this therapy, it is crucial to find a qualified practitioner and approach it with a consistent, structured plan. Rushing the process or using non-specialized resources can limit its effectiveness.
- Seek a Trained Professional: Look for a clinical hypnotherapist or psychologist who is specifically certified in gut-directed protocols. Their expertise ensures the suggestions are targeted correctly for digestive health.
- Practice Consistently: The benefits of GDH build over time. Most protocols involve a series of sessions, often supplemented with daily self-hypnosis recordings to reinforce the therapeutic suggestions between appointments.
- Explore Digital Options: For those who cannot access a therapist, digital programs have emerged as a validated alternative. The Nerva app, developed in collaboration with Monash University, provides a structured GDH program that has been shown in clinical trials to be effective for managing IBS symptoms.
- Maintain Realistic Expectations: Improvement is often gradual rather than immediate. Consistent practice and patience are key to achieving long-term symptom control and improved quality of life.
Top 7 IBS Remedies Comparison
| Item | Implementation Complexity 🔄 | Resource Requirements ⚡ | Expected Outcomes 📊 | Ideal Use Cases 💡 | Key Advantages ⭐ |
|---|---|---|---|---|---|
| Low FODMAP Diet | Moderate to high: requires strict 2-6 week elimination and reintroduction phases | High: needs dietitian support, meal planning, food tracking | High: 70-80% symptom improvement in bloating, gas, abdominal pain | IBS with food-triggered symptoms; identifying specific triggers | Scientifically validated, personalized dietary management |
| Peppermint Oil Supplements | Low complexity: oral capsules, simple dosing | Low: OTC availability, inexpensive | Moderate: ~40% symptom reduction in 2-4 weeks | IBS with abdominal pain and cramping; natural antispasmodic alternative | Well-studied, natural, few side effects |
| Probiotics (Multi-strain) | Moderate: consistent daily use for 4-12 weeks, some strain selection needed | Moderate: purchase of quality, refrigerated products recommended | Variable: symptom improvement over weeks, depends on individual | IBS with microbiome imbalance; broad symptom relief | Multiple strains improve gut balance, immune support |
| Psyllium Husk Fiber Supplementation | Low: simple daily intake with water, gradual increase recommended | Low: widely available, inexpensive | Moderate: improved bowel regularity, symptom relief | IBS with constipation or diarrhea; bowel normalization | Effective for multiple IBS subtypes, additional cholesterol benefits |
| Stress Management & CBT | High: 8-12 weeks structured therapy, patient engagement required | High: access to trained therapists or online apps | High: 6-12 weeks to significant symptom and quality of life improvement | IBS exacerbated by stress/anxiety; psychological symptom triggers | Long-lasting effects, no drug side effects |
| Regular Physical Exercise | Low to moderate: consistent 3-5 times/week activity, low barriers | Low: free or low-cost, no special equipment needed | Moderate: symptom reduction and improved gut motility | IBS with stress-related symptoms or constipation; overall health boost | Multiple health benefits, natural stress relief |
| Gut-Directed Hypnotherapy | High: 7-12 sessions with trained hypnotherapist, time-intensive | High: specialized therapists needed, possible cost | High: 70-80% significant symptom improvement, lasting effects | IBS refractory to other treatments; gut-brain axis related symptoms | Excellent long-term results, no side effects |
Crafting Your Personalized IBS Management Plan
Navigating the landscape of Irritable Bowel Syndrome can feel like a complex and often frustrating puzzle. Throughout this guide, we've explored a diverse toolkit of the best remedies for IBS, each backed by scientific evidence and real-world success. From the structured dietary precision of the Low FODMAP diet to the targeted relief offered by peppermint oil, and the foundational support of probiotics and psyllium husk, you now have a comprehensive overview of powerful, actionable strategies.
But the journey doesn't stop with diet and supplements. We've also highlighted the profound connection between the mind and the gut, emphasizing how stress management techniques like Cognitive Behavioral Therapy (CBT) and gut-directed hypnotherapy can fundamentally change your relationship with your symptoms. Paired with the consistent, gentle benefits of regular physical exercise, these remedies form a holistic framework for reclaiming control over your digestive health.
The Power of a Multi-faceted, Individualized Approach
The most critical takeaway is that there is no single magic bullet for IBS. Your path to relief is deeply personal. What works wonders for one person may have a minimal effect on another. This is why a methodical, patient, and personalized strategy is not just recommended; it's essential. The true power lies in strategically combining these remedies to create a synergistic effect that addresses your specific symptom profile, whether it's IBS-D, IBS-C, or mixed-type IBS.
Consider this your personalized roadmap:
- Start with a Foundation: Begin by addressing the core pillars of diet and stress. You might start with a modified Low FODMAP diet to identify trigger foods while simultaneously implementing a daily 10-minute mindfulness practice.
- Introduce Remedies Systematically: Avoid the temptation to try everything at once. Introduce one new supplement, like psyllium husk or peppermint oil, at a time. This allows you to accurately track its impact and determine if it's a valuable addition to your regimen. Keep a detailed symptom journal to monitor changes in bloating, pain, and bowel habits.
- Listen to Your Body's Feedback: Your body provides constant feedback. Pay close attention to how you feel after meals, after exercise, and during periods of stress. This self-awareness is your most powerful tool for refining your management plan over time.
Building Your Support System for Long-Term Success
You do not have to navigate this journey alone. Assembling a dedicated healthcare team is a crucial step toward sustainable relief. A gastroenterologist can provide an accurate diagnosis and rule out other conditions, while a registered dietitian can offer expert guidance through complex dietary changes like the Low FODMAP diet. In fact, for many, professional help in meal planning is a game-changer. Services dedicated to creating customized menus for dietary restrictions can remove the guesswork and stress, ensuring your nutritional needs are met while you heal.
Furthermore, integrating a practitioner who understands both conventional and traditional medicine can provide a more comprehensive perspective. An integrative specialist can help weave together dietary advice, mind-body therapies, and complementary treatments like acupuncture to create a truly holistic plan. By embracing this proactive, multi-layered approach, you transform from a passive sufferer into the active architect of your own well-being. Finding the best remedies for IBS is a process of discovery, and with these tools, you are well-equipped to build a life with greater comfort, predictability, and digestive peace.
Ready to take the next step with a personalized, integrative approach? At Eric Tsai Acupuncture and Herbs, we specialize in creating holistic treatment plans that combine the wisdom of Traditional Chinese Medicine with modern health strategies to address the root causes of digestive disorders like IBS. Visit Eric Tsai Acupuncture and Herbs to learn how our tailored acupuncture and herbal medicine protocols can become a cornerstone of your digestive wellness journey.