When medication isn't enough, alternative therapies for chronic pain open up a different path. The focus shifts to treating the whole person to manage that persistent discomfort.
These approaches are all about getting to the root causes, aiming to reduce inflammation and improve your quality of life through methods like acupuncture, mindfulness, and targeted physical therapies. It’s a move toward a more sustainable and empowering way to manage your health.
Rethinking Chronic Pain Management
Chronic pain is far more than just a symptom that overstays its welcome; it’s a complex condition that can actually rewire your nervous system. Think of it like a smoke alarm that keeps blaring long after the fire is out. The immediate danger is gone, but the alarm is stuck in the "on" position, disrupting every corner of your life.
This constant state of high alert is physically and emotionally draining, which is why so many people are starting to look for answers beyond the pharmacy counter.
The truth is, relying only on pharmaceuticals has its limits. While medication can be a critical tool, it often brings a host of side effects and the risk of dependency. More importantly, it can sometimes just mask the pain instead of addressing what's really causing it. This reality has sparked a growing interest in a more well-rounded strategy for wellness. To see the full scope of what's available, it's worth exploring the various complementary therapies that practitioners are using today.
The Broader Impact of Unmanaged Pain
The sheer scale of chronic pain is staggering. Globally, about 20% of adults live with it—that's more than 1.5 billion people.
In the United States alone, the condition costs the economy an estimated $600 billion every year in medical bills and lost productivity. These numbers underscore just how urgently we need better ways to manage pain.
But statistics don't tell the whole story. The personal toll is immeasurable, often touching every part of a person's life:
- Mental Health: Chronic pain is closely linked to higher rates of anxiety, depression, and social isolation.
- Physical Function: It can severely limit mobility and the ability to handle everyday tasks.
- Overall Well-being: Quality of sleep plummets, and with it, overall life satisfaction.
A New Perspective on Relief
This guide doesn't position alternative therapies as a replacement for conventional medicine. Instead, we see them as essential parts of a modern, comprehensive pain management plan. This approach is often called integrative medicine, and it blends the best of both worlds to create a strategy tailored to you.
An integrative model empowers you to take an active role in your healing journey. It’s about building a toolbox of strategies—from mindfulness to acupuncture—that allows you to reclaim a sense of control over your body and your life.
By exploring these options, you open the door to a more hopeful and sustainable way to find relief. The goal is to get past just managing symptoms and start building a real foundation for long-term health and vitality. Our article on what is integrative medicine offers a deeper dive into this collaborative approach to healthcare. It’s all about finding what truly works for you.
Tapping into the Mind-Body Connection for Pain Control

When you're dealing with chronic pain, it's easy to feel like your mind and body are at war. But what if I told you your mind could be your most powerful ally? The brain isn't just a passive receiver of pain signals; it actively interprets and can even amplify or dial them down.
Think of your brain as the soundboard in a recording studio. It has controls that adjust the volume, bass, and treble of every pain signal it receives. Mind-body therapies are all about learning how to operate that soundboard yourself. By training your brain to reinterpret or turn down the intensity of those signals, you can fundamentally change how you experience pain. It's an approach that puts you back in the driver's seat.
This isn't just a niche idea anymore. It's gaining serious traction in mainstream medicine. In fact, major institutions like the U.S. Veterans Health Administration now recommend non-drug treatments—including yoga, mindfulness, and cognitive behavioral therapy—as first-line options for managing pain. This shift underscores a move toward strategies that reduce opioid reliance and genuinely improve a person's quality of life. You can read more about these recommendations for pain management and see the data for yourself.
Understanding Cognitive Behavioral Therapy
Cognitive Behavioral Therapy (CBT) is a structured, goal-oriented form of talk therapy that helps you untangle the negative thoughts and behaviors wrapped around your pain. The core idea is simple but profound: your thoughts, feelings, and physical sensations are all deeply connected.
For instance, someone with chronic back pain might think, "This is unbearable, I'll never be able to play with my kids again." This thought can quickly spiral into despair and anxiety, which physically causes muscles to tense up, making the pain even worse. It's a vicious cycle. CBT gives you the tools to break it.
A CBT therapist helps you to:
- Spot Distorted Thinking: You learn to catch those automatic negative thoughts in the act.
- Challenge Limiting Beliefs: You start questioning the evidence for and against your pain-related assumptions.
- Build a Coping Toolkit: You develop practical skills, from relaxation exercises to activity pacing, to handle flare-ups with more confidence.
CBT is especially powerful for conditions where psychological distress pours fuel on the fire, like fibromyalgia, chronic headaches, and arthritis. It doesn't erase the source of the pain, but it equips you to manage its impact on your life.
The Power of Mindfulness and Meditation
Mindfulness-Based Stress Reduction (MBSR) takes a slightly different, yet equally powerful, approach. Where CBT focuses on changing your thoughts, mindfulness teaches you to observe them—and your physical sensations—without judgment. The goal is to create a bit of space between you and the pain.
Imagine your pain is a loud, blaring radio you can't turn off. Instead of trying to smash it, mindfulness teaches you to simply acknowledge the noise, notice its qualities, and then gently shift your focus to other things in the room—the feeling of your breath, the support of your chair, or the quiet hum of an appliance.
A common mindfulness practice is the "body scan" meditation. Here, you systematically guide your awareness through different parts of your body, simply noticing any sensations—tingling, warmth, or even pain—without trying to fix them. This practice helps rewire the brain to be less reactive to pain signals over time.
The stress-reduction benefits are a huge piece of the puzzle. Chronic pain often keeps the body stuck in "fight or flight" mode, flooding it with stress hormones that can increase inflammation and pain sensitivity. Mindfulness helps calm that storm. Learning how to cope with stress is a non-negotiable part of any long-term pain management plan.
Therapeutic Yoga and Gentle Movement
Therapeutic yoga blends physical postures, controlled breathing, and meditation to improve both physical function and mental calm. This is a far cry from a fast-paced fitness class; the entire practice is built around adapting poses to work with your body's limitations, not against them.
The benefits for chronic pain come from several angles:
- Increased Flexibility and Strength: Gentle stretching can ease muscle tension around sore joints, while building strength in supporting muscles improves stability and takes off some of the load.
- Improved Body Awareness: Yoga helps you get back in tune with your body’s signals, making it easier to tell the difference between the "good pain" of a productive stretch and the "bad pain" of an injury.
- A Calmer Nervous System: The focus on deep, slow breathing activates the body's "rest and digest" response, which is a natural antidote to stress and heightened pain perception.
Therapeutic yoga has shown remarkable benefits for people with chronic low-back pain, arthritis, and fibromyalgia. It provides a safe and supportive way to re-engage with movement, helping you rebuild trust in your body and conquer the fear that so often accompanies chronic pain.
Exploring Hands-On Physical Therapies
While your mind is a powerful ally in managing pain, sometimes the most direct route to relief is a physical one. Hands-on therapies work by getting to the root of the problem—addressing the body's structure, systems, and energy pathways to restore balance and dial down discomfort.
These treatments aren't about just covering up symptoms. Instead, they operate on a simple but profound principle: the body has an incredible, innate ability to heal itself. Therapies like acupuncture, chiropractic care, and massage are all designed to kickstart that natural process by targeting the physical source of the pain.
The growing popularity of these methods is backed by solid results. For example, recent findings on traditional Chinese medicine show significant improvements for people with tough conditions like rheumatoid arthritis and peripheral neuropathy, leading to better hand mobility, stronger grip, and an overall better quality of life.
Acupuncture: Rebalancing the Body’s Energy
Acupuncture is an ancient practice built on the concept of balancing the body's vital energy, known as "qi" (pronounced "chee"). The idea is that qi flows through the body along specific pathways. When that flow gets blocked or disrupted, it can lead to pain and illness.
To get things moving again, a licensed acupuncturist inserts hair-thin, sterile needles into very specific points on the body. This isn't just theory; modern science is catching up. Research suggests these needles stimulate nerves, muscles, and connective tissues, which in turn boosts the production of endorphins—your body's own natural painkillers. It can also influence how your brain actually perceives and processes pain signals.
Think of it like a traffic jam on a highway. The pain is the gridlock. Acupuncture needles act like traffic controllers, placed at key intersections to clear the blockage and get everything flowing smoothly again, restoring communication and function.
Acupuncture is a go-to for a wide range of chronic pain conditions, including:
- Low back pain
- Neck pain
- Migraines and tension headaches
- Pain from osteoarthritis
Many people find the sessions deeply relaxing. To get a better feel for how it works in practice, our detailed guide on acupuncture for chronic pain breaks down the mechanics and benefits.
Chiropractic Care: Aligning Your Structure for Relief
Chiropractic care focuses on the crucial link between your body's structure—mainly the spine—and how it functions as a whole. The central idea is that when your musculoskeletal system is properly aligned, your body is much better equipped to heal itself without needing drugs or surgery.
When the vertebrae in your spine get out of place (a condition chiropractors call a subluxation), they can put pressure on the surrounding nerves. This nerve interference can trigger pain not just in your back, but in seemingly unrelated parts of your body.
A chiropractor uses their hands or specialized tools to apply a controlled, quick force to a spinal joint. This "adjustment" is meant to improve your spine's mobility and get your body working properly again. It's not just about adjustments, though. A good chiropractor often includes soft-tissue therapy, targeted exercises, and lifestyle advice in their treatment plans.
Chiropractic is especially helpful for mechanical pain issues like:
- Chronic low-back and neck pain
- Sciatica (that sharp nerve pain shooting down the leg)
- Certain headaches that stem from neck tension
The end goal is always to improve your mobility, calm down nerve irritation, and get your joints and muscles back to doing their job.
Massage Therapy: Releasing Deep-Seated Tension
Therapeutic massage is so much more than a spa day indulgence. It's a clinical, hands-on approach to working with the body's soft tissues—your muscles, connective tissues, tendons, and ligaments. By using different types of pressure and movement, a skilled massage therapist can target the very source of chronic pain.
The magic happens on two levels. Physically, massage boosts blood and oxygen flow to tight, knotted muscles, which helps wash away soreness and inflammation. At the same time, it has a powerful effect on your nervous system, helping to lower stress hormones like cortisol while increasing mood-lifters like serotonin and dopamine.
This infographic shows the average pain reduction reported from several mind-body therapies, which are often used alongside hands-on treatments.
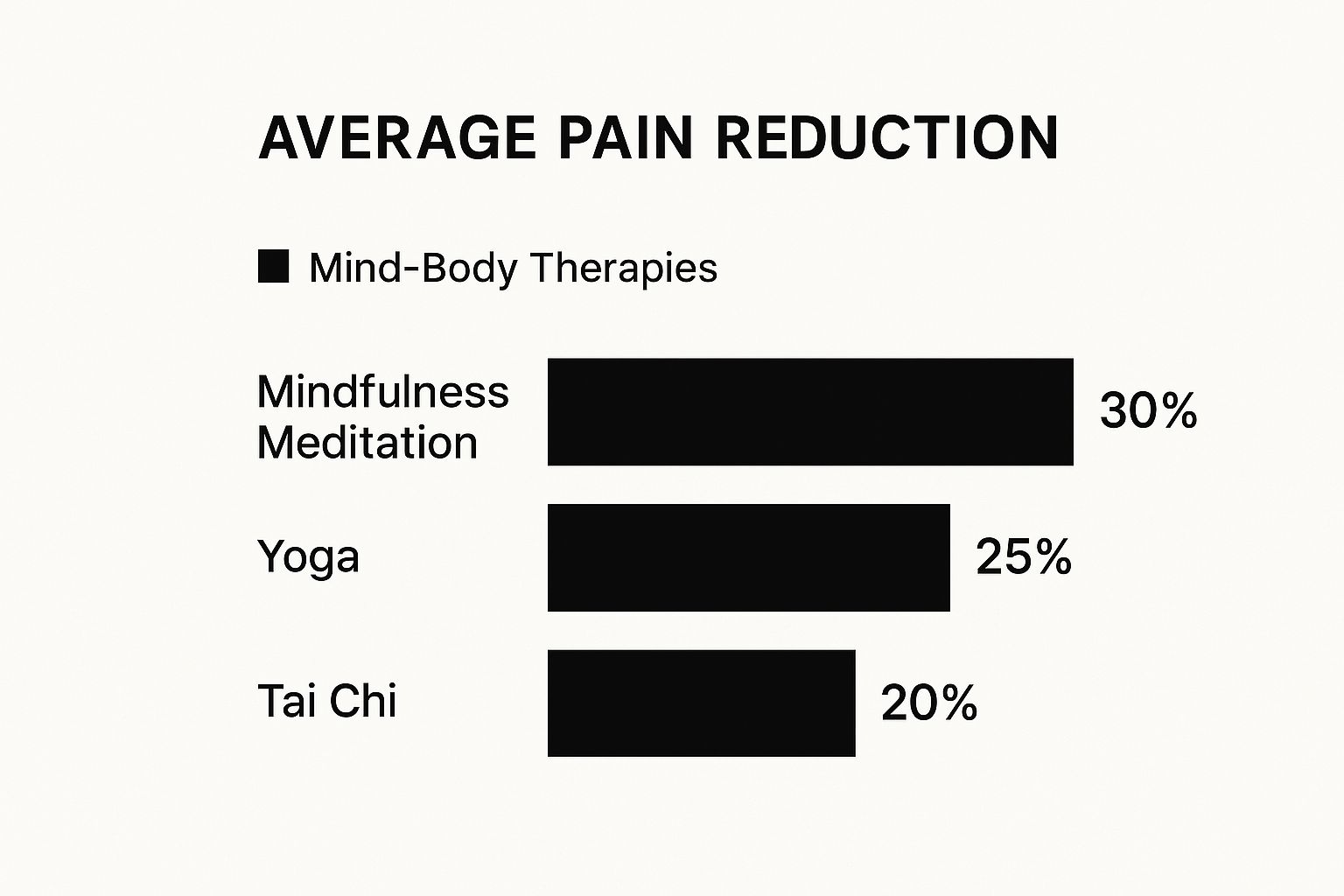
The numbers show that different approaches can bring significant relief, which really drives home the point that finding the right therapy for your specific pain is key.
Different styles of massage tackle different problems. For instance, deep tissue massage goes after chronic muscle knots, while myofascial release focuses on the web of connective tissue surrounding your muscles. Massage can be a game-changer for conditions like fibromyalgia, stubborn shoulder pain, and osteoarthritis.
Comparing Popular Physical Therapies for Chronic Pain
Choosing between acupuncture, chiropractic, and massage can feel overwhelming. It really boils down to your specific condition, the type of pain you're experiencing, and what you're comfortable with.
This quick-reference guide can help you compare these major therapies at a glance.
| Therapy | Primary Goal | Core Technique | Best For Conditions Like |
|---|---|---|---|
| Acupuncture | Restore the flow of the body's natural energy (qi) and stimulate its self-healing mechanisms. | Inserting fine, sterile needles into specific points along the body's energy pathways. | Migraines, low-back pain, osteoarthritis, and nerve-related pain. |
| Chiropractic Care | Correct spinal and joint misalignments to reduce pressure on nerves and improve overall function. | Applying controlled, specific "adjustments" to joints, particularly those of the spine. | Mechanical back and neck pain, sciatica, and tension headaches. |
| Massage Therapy | Release muscle tension, reduce inflammation, and calm the nervous system by manipulating soft tissues. | Kneading, tapping, and applying pressure to muscles and connective tissues. | Fibromyalgia, muscle soreness, soft-tissue injuries, and stress-related pain. |
Ultimately, the best therapy is the one that addresses the root cause of your pain and helps you regain function and quality of life. Sometimes, a combination of approaches works best.
Using Natural Remedies and Supplements Safely

Aside from physical therapies and mental practices, many people explore the world of natural remedies and dietary supplements to get a handle on chronic pain. The appeal is understandable—these options often come from plants and can feel like a gentler, more holistic way to find relief.
But it’s important to walk this path with a healthy dose of both optimism and caution. The word “natural” doesn’t automatically mean “safe,” especially if you’re already taking other medications.
These remedies can be powerful allies, but they can also clash with prescriptions, trigger side effects, or simply not work if used incorrectly. That’s why talking to your doctor or another qualified healthcare provider isn't just a suggestion; it's a must before you add any new supplement to your daily routine.
Navigating the World of Supplements
Unlike prescription drugs, the supplement industry isn’t held to the same strict regulatory standards. This means the quality, purity, and even the dosage can vary wildly from one brand to the next.
To make sure you’re getting what you paid for and protecting your health, you have to become a savvy consumer.
Here are a few essential steps to take:
- Look for Third-Party Testing: Prioritize products verified by independent organizations like NSF International, USP, or ConsumerLab.com. This seal of approval confirms the product contains what the label claims and is free from harmful contaminants.
- Start with a Low Dose: Always begin with the lowest recommended dose to see how your body reacts. You can always increase it later if needed, but you can’t undo a strong negative reaction.
- Consult a Professional: Your doctor or pharmacist is your best resource for checking potential drug interactions. This is a critical safety step that should never be skipped.
A Spotlight on Popular Pain-Relieving Remedies
Several natural compounds have rightfully earned a reputation for their pain-relieving and anti-inflammatory properties. Let's take a closer look at the science behind some of the most popular and well-researched options.
Turmeric and Curcumin
You probably know turmeric as the vibrant golden spice that gives curry its color. But its real power comes from a compound inside called curcumin. Think of curcumin as a natural agent that helps dial down the body's inflammatory response—a major driver of chronic pain, especially in conditions like osteoarthritis.
Studies have shown that curcumin can be as effective as some over-the-counter anti-inflammatory drugs for easing joint pain and stiffness, often with fewer stomach-related side effects. For it to work best, look for supplements that combine it with black pepper (piperine), which dramatically boosts its absorption.
Capsaicin: The Power of Chili Peppers
Capsaicin is the fiery compound in chili peppers that gives them their kick. When you apply it to your skin in a cream or patch, it creates a warming sensation that essentially distracts your nerves from sending pain signals up to your brain.
Over time, capsaicin can actually deplete a chemical messenger called "substance P," which is responsible for transmitting pain signals from nerve cells. In a way, it helps turn down the volume on pain communication right where you apply it.
This makes it a fantastic choice for localized pain, like arthritis in the hands and knees or the lingering nerve pain that can follow a shingles outbreak.
CBD (Cannabidiol)
Cannabidiol, better known as CBD, is a non-psychoactive compound from the cannabis plant that has become a major player in pain management. It works by interacting with the body’s endocannabinoid system, a complex network that helps regulate everything from pain and inflammation to mood and sleep.
Available as oils, creams, and edibles, CBD is reported by many to reduce not just their pain but also the anxiety that so often comes with it. As you investigate ways to manage discomfort, many people find success by exploring effective natural remedies for back pain and other chronic issues. Just remember, professional guidance is key to finding a safe and effective approach tailored to your unique health needs.
Building Your Personal Pain Management Plan

Knowing about the different non-drug therapies for chronic pain is one thing, but actually putting that knowledge to work is what makes a real difference. This is where you move from being a passenger in your healthcare journey to taking the driver's seat by creating a personal pain management plan.
This isn't about finding a single magic bullet. It’s about building a flexible, multi-faceted strategy that works for you and can change as your needs do.
Think of it like being the general manager of a sports team. You're assembling a roster of different specialists and strategies, and your plan is the playbook. It outlines your goals, who's on your team, and how you'll work together to manage your pain and get back to living a fuller life. The most effective plans almost always blend several therapies, creating a combined effect that's far more powerful than any single approach.
H3: Step 1: Become a Detective of Your Own Pain
Before you can create a winning strategy, you need to understand the opponent. That means you have to get to know your pain—its habits, its triggers, and its patterns. The best way to start is by keeping a detailed pain journal for a couple of weeks.
This simple act of tracking your symptoms can uncover surprising connections you might have missed. It also gives you solid data to share with your healthcare providers, which helps them make a more accurate diagnosis and recommend more effective treatments.
In your journal, try to capture:
- Pain Intensity: Rate your pain on a scale of 1-10 at different times of the day.
- Pain Character: What does it feel like? Is it a sharp stab, a dull ache, a burning sensation, or a throb?
- Triggers: What seems to kick it off or make it worse? Think about activities, foods, stress levels, or even the weather.
- Relievers: What makes it better? A hot bath? A short walk? A specific stretch?
- Time of Day: Is it a bigger problem when you first wake up or does it build up by the end of the day?
Once you have this information, you can set real, achievable goals. Instead of a fuzzy goal like "I want to feel better," you can aim for something concrete, like "I want to reduce my morning stiffness enough to walk the dog for 15 minutes without severe pain."
H3: Step 2: Find and Vet Your Practitioners
Once you have an idea of which therapies you want to try, the next hurdle is finding the right people to guide you. The skill and approach of your practitioner are just as crucial as the therapy itself. You're looking for someone who is not only an expert in their field but also a good listener and a true partner in your care.
A great place to start is by asking your primary care physician or other specialists you trust for referrals. They often have a network of professionals they've already vetted.
If you're searching on your own, here’s what to look for:
- Licensing and Certification: Make sure they hold the proper credentials from state or national boards (for example, the NCCAOM for acupuncturists).
- Experience: Don't be shy about asking how much experience they have treating your specific condition.
- A Collaborative Mindset: You want someone who is happy to work with your other doctors to create a cohesive, integrated care plan.
H3: Step 3: Assemble Your Integrative Care Team
Your primary doctor should always be the quarterback of your pain management team. It is absolutely essential to keep an open line of communication with them about any alternative therapies for chronic pain you're trying or even just thinking about.
An effective pain management plan requires a personalized approach that considers your preferences and unique medical needs. Keep an open dialogue with your physician to find the treatment best suited for you.
Your doctor can spot potential conflicts, like an herb that might interfere with a prescription medication, and ensure all your treatments are working together safely. This team-based approach, often called integrative medicine, turns your healthcare from a series of disconnected appointments into a single, coordinated effort focused on your well-being.
Remember, this communication goes both ways. When you keep your doctor in the loop about what’s working, you're not just helping yourself—you're also helping to educate them on the real-world benefits of these therapies. This helps the wider medical community gain a better appreciation for these powerful tools. From here, the final step is simply to keep track of what works and adjust as you go.
Setting Realistic Expectations for Your Journey
Taking charge of your chronic pain by exploring alternative therapies is a huge step forward. But to make it a successful one, it's really important to start with the right frame of mind. The biggest pitfall I see is the hope for a "magic bullet." The truth is, lasting relief isn't usually a lightning bolt moment; it’s a journey of gradual discovery.
Think of it like learning a new skill, maybe playing the guitar. In the beginning, your fingers are clumsy, and progress feels slow. You'll try different chords and techniques—some will click, and some just won't. That period of trial and error isn't a failure; it's a vital part of figuring out what truly works for you.
Reframing the Placebo Effect
I often hear patients worry that if a therapy helps, maybe it's "just the placebo effect." Instead of seeing this as a negative, I encourage them to reframe it as proof of the powerful connection between mind and body. The placebo effect isn't just in your head; it’s a real, measurable physiological response that shows how much influence your brain has over your physical health.
When you truly believe a treatment can help, your brain can actually release its own natural painkillers, like endorphins, and dial down the stress hormones that make pain feel so much worse.
The placebo response doesn't invalidate a therapy; it proves that your mindset is an active ingredient in your own healing. Learning to harness this through positive expectation isn't a sign of weakness—it's a smart strategy that puts you back in the driver's seat.
Embracing Patience and Persistence
Ultimately, finding what works takes time and patience. Some therapies need a few weeks or even months to show their full potential, while others work best when you combine them. Considering that around 65% of adults over 65 live with chronic pain, it's clear this is a common and often long-term challenge.
The real key here is resilience. You're going to have good days and bad days—that’s just part of the process. The goal isn't to find one perfect, all-encompassing cure. It's about building a personal toolkit of strategies that, over time, consistently makes your life better. If you can manage your expectations and celebrate the small wins, you'll bring the optimism and strength you need to succeed in the long run.
Your Questions, Answered
Stepping into the world of non-pharmaceutical pain therapies can feel like learning a new language. You probably have a lot of practical questions, and that's completely normal. Getting clear on things like insurance, finding the right person to work with, and how these therapies fit with your current medical care is a critical part of the process.
Let's walk through some of the most common questions people ask as they start this journey.
Will My Insurance Cover These Therapies?
This is the big question, and the honest answer is: it depends. The landscape of insurance coverage is slowly changing, and some plans are now covering treatments like chiropractic care and acupuncture, especially for specific conditions. On the other hand, therapies like massage or herbal medicine are often paid for out-of-pocket.
The single most important thing you can do is call your insurance provider directly before you start any new treatment. You'll want to ask about your specific plan's benefits. Find out if you need a referral from your doctor or if there's a cap on how many sessions they'll cover each year. Getting these details sorted out first can save you from a lot of financial headaches down the road.
How Can I Find a Good Practitioner?
Finding a qualified and trustworthy professional is non-negotiable. Your safety and the effectiveness of your treatment depend on it.
A great place to start is by asking for a referral from your primary care doctor or specialist. They often have a network of practitioners they know and trust.
If you're searching on your own, always look for someone who is properly licensed or certified by a recognized state or national board.
Your first meeting is a two-way interview. Don't be shy about asking questions. A good practitioner will be happy to discuss their experience with your specific condition and explain how they plan to work alongside your other doctors.
Can I Use These Therapies Along With My Regular Medical Treatments?
Absolutely. In fact, this is often the most effective approach. We call it "integrative" or "multimodal" care. Think of it as building a team where each member brings a unique skill to help you manage pain from different angles.
The key here is communication. It's crucial that this is done with the full knowledge and guidance of your entire healthcare team. Your primary doctor must be kept in the loop about every therapy you're trying—including any supplements—to make sure everything works together safely and effectively.
Ready to build a pain management plan that’s right for you? At Eric Tsai Acupuncture and Herbs, we blend the best of traditional wisdom and modern knowledge to help you find relief that lasts. Learn more and schedule your consultation today.