When you're looking for a natural path to manage endometriosis, it's about so much more than just supplements or a specific diet. The most effective approach is a comprehensive one that weaves together anti-inflammatory eating, mindful movement, stress management, and targeted supplementation to create real, lasting change.
This isn't a quick fix, but a realistic, evidence-informed roadmap designed to help you calm your body's inflammatory response, balance your hormones, and ultimately, get your life back.
Understanding Endometriosis and Your Body
Living with endometriosis often feels like a full-body experience, impacting everything from your energy and mood to your ability to get through the day. While the clinical definition is tissue similar to the uterine lining growing where it shouldn't, what you experience is a complex storm of inflammation, hormonal shifts, and an immune system in overdrive.
This is precisely why a natural, whole-body approach can be so powerful. Instead of just chasing symptoms, you’re getting to the root of the problem. We’re aiming to douse the underlying fire of inflammation that drives both the pain and the growth of endometrial lesions, while also supporting your body's ability to metabolize hormones—a critical piece of the endo puzzle.
The Core Pillars of Natural Management
When tackling endometriosis from a natural perspective, I find it helps to frame the strategy around a few core pillars. Think of these as the foundational areas where consistent, sustainable changes will give you the most significant results. They all work together, creating a powerful synergistic effect that builds your body's resilience over time.
This table breaks down the essential pillars we'll be covering in this guide.
Core Pillars of Natural Endometriosis Management
| Pillar | Primary Goal | Key Actions |
|---|---|---|
| Inflammation Control | Reduce systemic inflammation to decrease pain and lesion activity. | Adopt an anti-inflammatory diet, incorporate specific supplements like omega-3s and curcumin. |
| Hormonal Balance | Support healthy estrogen metabolism and promote progesterone balance. | Focus on gut health, liver support, and minimize exposure to endocrine disruptors. |
| Immune System Support | Modulate the immune response to manage inflammation and abnormal tissue growth. | Prioritize sleep, manage stress, and ensure adequate intake of key nutrients like Vitamin D and zinc. |
| Pain & Symptom Relief | Directly address pelvic pain, bloating, and other common symptoms. | Utilize pelvic floor therapy, acupuncture, herbal medicine, and targeted movement. |
Each of these pillars represents a crucial component of a holistic plan. By addressing them together, you create a much more stable and resilient internal environment.
- Inflammation Control: This is ground zero. Our primary goal is to lower the systemic inflammation that contributes so heavily to the pain and activity of the lesions.
- Hormonal Balance: Here, we focus on helping your body process estrogen efficiently and promoting healthy progesterone levels to counteract estrogen dominance. A big part of this is learning to spot and avoid common hormone-disrupting chemicals. This resource on the 5 most common hormone disruptors in daily life and their impact on women's health is a great place to start.
- Immune System Support: A balanced, well-functioning immune system is absolutely essential for managing the inflammatory cascade and helping the body recognize abnormal tissue.
From a Traditional Chinese Medicine (TCM) perspective, the severe, stabbing, and fixed pain so characteristic of endometriosis often points to a pattern we call Blood Stasis. In simple terms, this means circulation in the pelvic area is stuck or impaired, leading to blockages that create pain and allow tissue to accumulate. You can learn more about what Blood Stasis is and how it relates to pain in this detailed breakdown.
Think of this guide as a practical, compassionate partner on your journey. It’s not about achieving perfection or following restrictive rules. It's about empowering you with the knowledge to make informed, nurturing choices for your body that bring you closer to genuine, lasting relief.
Your Anti-Inflammatory Endometriosis Diet

When you're dealing with endometriosis, food is one of the most powerful and immediate tools you have to influence how you feel. It's not about restriction or creating a joyless relationship with eating. Instead, think of it as a strategic way to make nourishing choices that actively work for your body, not against it.
What you eat can either fan the flames of inflammation and hormonal chaos or help calm the entire system down. Since endometriosis is driven by inflammation and fueled by estrogen, our dietary approach has two clear goals: cool off systemic inflammation and support healthy estrogen balance.
By loading your plate with anti-inflammatory foods, you can directly impact the pain signals and inflammatory pathways that trigger your symptoms. At the same time, we need to support the body’s natural detox crew—your liver and digestive system—to help them clear out excess estrogen effectively.
Building Your Anti-Inflammatory Foundation
The core of this approach is shifting toward whole, unprocessed foods packed with nutrients and antioxidants. Your grocery cart really is your first line of defense.
A great place to start is with healthy fats, especially omega-3 fatty acids. I can't overstate how important these are. Omega-3s are the building blocks for powerful anti-inflammatory compounds in your body called prostaglandins, and studies consistently link higher intake with reduced endometriosis risk and symptoms.
- Fatty Fish: Aim for two or three servings a week of salmon, mackerel, sardines, or anchovies.
- Plant-Based Powerhouses: Flaxseeds (make sure they're ground), chia seeds, and walnuts are fantastic. It’s easy to sprinkle them on oatmeal, blend them into smoothies, or toss them into a salad every day.
From there, it's all about color. Pile your plate high with a rainbow of fruits and vegetables. They deliver a knockout punch of antioxidants to fight oxidative stress—a key driver of endo-related inflammation—and the fiber needed for hormone balance.
The Critical Role of Fiber and Gut Health
For anyone with endometriosis, fiber is absolutely non-negotiable. It has a crucial dual role: it binds to excess estrogen in your gut, ensuring it gets escorted out of your body instead of being reabsorbed into circulation. A healthy gut is the cornerstone of hormonal health, and fiber is the superfood for the good bacteria that keep things running smoothly.
Many of my clients with endo also struggle with gut issues like painful bloating, so supporting your digestive tract can bring tremendous relief. For a deeper dive, learning about the best foods for leaky gut can be a game-changer for your overall wellness.
Key Takeaway: Your goal should be at least 25-30 grams of fiber every day. You'll find it in leafy greens, berries, cruciferous veggies (like broccoli and cauliflower), legumes, and whole grains like quinoa and oats.
Foods to Reduce or Avoid
What you choose to limit is just as important as what you add. Some common foods are notorious for promoting inflammation and can make symptoms significantly worse.
- Processed Foods & Refined Sugars: These are major inflammation drivers. Think sugary drinks, packaged snacks, white bread, and pastries.
- Red Meat: Some research points to a link between high consumption of red meat and an increased risk of endometriosis. It’s wise to limit it, especially processed versions like bacon and sausage.
- Trans Fats: Found in many fried foods, margarines, and packaged baked goods, these are highly inflammatory and should be avoided completely.
This can feel like a big shift, so start small. Try swapping one processed snack for an apple or choosing grilled salmon over a burger for dinner. Small changes add up.
Exploring Gluten and Dairy Sensitivities
The conversation around gluten and dairy is a big one in the endo community, and for good reason. While not everyone needs to eliminate them, many women report a dramatic improvement in their symptoms after doing so. One compelling study found that 75% of participants experienced less pain after going on a gluten-free diet for 12 months.
The thinking here is that for some people, these proteins can trigger a low-grade inflammatory or immune response, adding more fuel to the fire. If you suspect they might be a problem for you, a structured elimination diet is the best way to find out for sure.
- Eliminate: Remove all gluten or dairy (or both) from your diet for at least four full weeks. This requires careful label reading, but it's worth it.
- Observe: Keep a simple journal. Note your pain levels, energy, bloating, and other key symptoms during this time.
- Reintroduce: After the four weeks, bring one food group back in and see how your body reacts over the next 72 hours. Any return of symptoms is a clear sign.
This process gives you clear, personalized answers about what your body needs. It’s about empowerment, not deprivation. And with so many amazing alternatives like almond milk and quinoa pasta available today, making the switch is easier than ever.
Movement and Pelvic Floor Physical Therapy

When you're living with chronic pain, the very thought of exercise can feel impossible. But what if we reframe "exercise" as gentle, restorative movement? This shift in perspective is a powerful tool for managing endometriosis. It’s not about pushing through pain in a high-intensity workout; it’s about choosing activities that reduce inflammation, soothe tension, and support a healthier hormonal environment.
The right kind of movement boosts blood flow to the pelvic region, which can ease pain and break up stagnation. It also cues your body to release endorphins—its own natural pain-relievers—and helps keep symptom-worsening stress hormones in check. Think of it as moving with your body, not against it.
And the research backs this up. One recent study showed that women with endometriosis who engaged in regular physical activity, like aerobic training and even brisk walking, saw a major improvement in their quality of life and a significant reduction in pain. The participants in the moderate exercise group reported a 30-40% decrease in pain severity and a 25% improvement in their overall well-being. You can dive deeper into these promising exercise findings yourself.
Gentle Exercises to Soothe Your Body
The key is finding movement that feels good to your body. Since high-impact exercise can sometimes trigger a flare-up, the goal is to focus on activities that build strength and flexibility without jarring your system.
- Mindful Yoga: Gentle or restorative yoga is fantastic for endometriosis. Poses like Cat-Cow, Child's Pose, and gentle spinal twists are especially helpful for releasing the deep-seated tension that builds up in the pelvic floor, hips, and lower back.
- Swimming and Water Aerobics: The buoyancy of water is a gift. It supports your body, taking all the pressure off your joints and pelvic area while the gentle resistance still provides a great workout.
- Walking: Never underestimate the power of a simple walk. It gets your circulation going, lifts your mood, and is incredibly easy to fit into your day.
- Stretching: Focus your stretching on opening the hips and releasing tight muscles in the lower back and abdomen. This directly counteracts the chronic clenching and tightness that comes with pelvic pain.
The goal is consistency over intensity. Even 15-20 minutes of gentle movement most days of the week can make a profound difference in your pain levels and overall energy.
The Game-Changing Role of Pelvic Floor Therapy
This might be one of the most important—and often overlooked—therapies for endometriosis. The condition is so much more than just the endometrial-like lesions. The constant inflammation and pain signals cause the muscles of the pelvic floor to go into a state of chronic tightness, a condition called hypertonicity.
This muscle tension becomes a significant pain generator on its own, contributing to painful sex, bladder urgency, and that nagging lower back ache. A pelvic floor physical therapist (PFPT) is a specialist trained to address this exact problem. They use gentle, hands-on techniques to release these wound-up muscles, work on adhesions, and retrain your body to function without pain.
A skilled therapist will often apply the principles of movement analysis to figure out your body's unique patterns and build a care plan that’s truly personalized.
What to Expect from Pelvic Floor PT
Seeing a pelvic floor therapist is an incredibly proactive step. Here’s a glimpse of what the journey often looks like:
- A Detailed Assessment: Your first visit is all about understanding you. Expect a deep dive into your symptoms and medical history, followed by a gentle external and internal exam to pinpoint muscle tone, trigger points, and functional issues.
- Manual Therapy: Your therapist will use skilled, hands-on techniques to release tight trigger points in the muscles of your pelvic floor, abdomen, hips, and back.
- Personalized Exercises: You’ll leave with a toolkit of specific stretches and relaxation exercises to do at home. A cornerstone of this is often diaphragmatic breathing (or "belly breathing"), which is a powerful way to calm the nervous system and relax the pelvic floor.
- Education: You'll learn a ton about your own body and how pain cycles work. This knowledge is empowering, giving you the tools to manage symptoms for the long haul.
Finding a therapist who specializes in pelvic pain is non-negotiable. They bring a level of understanding and compassion that is essential for navigating the complexities of endometriosis and finding lasting relief.
Acupuncture and Herbal Medicine for Endometriosis

Beyond diet and lifestyle adjustments, we find powerful allies in ancient healing practices like acupuncture and herbal medicine. Far from being just "feel-good" therapies, these are sophisticated systems of medicine that have gained significant modern recognition for their role in managing endometriosis symptoms. They work by influencing pain pathways, helping to regulate hormones, and calming an overactive nervous system, offering a robust, evidence-backed way to treat endometriosis naturally.
From a Traditional Chinese Medicine (TCM) lens, endometriosis is often understood as a condition of "Blood Stasis" in the lower abdomen. This isn't literal, but rather a concept describing poor circulation that leads to the accumulation of tissue and the sharp, fixed, and debilitating pain so characteristic of this condition. The entire goal of treatment, then, is to get things moving again—to invigorate circulation, clear that stagnation, and soothe the root imbalances driving the symptoms.
How Acupuncture Actually Addresses Endometriosis Pain
Acupuncture involves placing ultra-fine, sterile needles at very specific points on the body. This isn't just a placebo; the practice prompts very real physiological changes that can bring profound relief from endometriosis pain.
Modern research has shown that acupuncture stimulates nerves, sending signals to the brain that trigger the release of endorphins—your body’s own powerful pain-killing chemicals. It also helps down-regulate the sympathetic nervous system (your "fight-or-flight" response), which is often stuck in overdrive when you're living with chronic pain. This calming effect is key, as it can reduce overall muscle tension and lower systemic inflammation.
A licensed acupuncturist won’t just focus on your pelvic pain. They’ll create a personalized treatment plan based on your unique pattern of symptoms, addressing related issues like digestive upset, fatigue, and menstrual irregularities. It’s a true whole-system approach.
Some of the most compelling research comes from combining acupuncture with moxibustion, a technique where an herb (mugwort) is gently and safely burned near the skin to create a deep, penetrating warmth that enhances circulation. One remarkable study found that after several months of this combination therapy, 42 out of 72 patients became pregnant. The overall effective rate for symptom improvement was an incredible 93.05%. You can read the full research about these endometriosis findings for yourself.
Tapping into the Power of Herbal Medicine
Herbal medicine is the other key pillar of TCM and works hand-in-hand with acupuncture. Rather than prescribing a single herb, practitioners formulate custom blends of botanicals where each ingredient plays a specific role—some reduce pain, others move blood, and some help modulate hormones.
These aren't quaint folk remedies. Many of these herbs contain potent bioactive compounds that have been clinically studied for their anti-inflammatory, analgesic, and hormone-balancing effects. While they can be incredibly effective, they are also powerful medicine.
Here are a few classic formulas often used in cases of endometriosis:
- Gui Zhi Fu Ling Wan: A cornerstone formula for pelvic masses and painful periods linked to Blood Stasis. It's specifically designed to invigorate circulation and break down accumulations.
- Chai Hu Shu Gan San: This formula is a game-changer when stress and emotional frustration make your symptoms flare up. It helps smooth the flow of Qi (energy) and calms the nervous system, which can dramatically ease premenstrual tension and pain.
- Dang Gui Shao Yao San: A deeply nourishing formula used when underlying deficiencies contribute to pain and irregular cycles. It focuses on building blood while harmonizing the liver and spleen. For a deeper dive into botanicals, explore our guide on the best herbs for hormone balance.
Finding a Qualified and Safe Practitioner
This is the most critical piece of advice I can give: never self-prescribe herbs or get acupuncture from an untrained individual. The effectiveness and, more importantly, the safety of these therapies hinge entirely on the skill and knowledge of your provider.
Look for a practitioner who is licensed in your state (often designated as L.Ac. for Licensed Acupuncturist) and holds a master's or doctoral degree in Acupuncture and Oriental Medicine. This credentialing ensures they have undergone thousands of hours of rigorous training in both diagnosis and safe application.
A qualified herbalist will always conduct a thorough intake and ask about your current medications to rule out any potential negative interactions. Your treatment should be personalized, safe, and part of a collaborative relationship focused on your long-term health and well-being.
Taming Stress and Prioritizing Sleep for Hormonal Balance
Living with chronic pain is, by its very nature, stressful. But this isn't just an emotional weight—the stress itself can kick off a vicious cycle that makes endometriosis symptoms significantly worse. When you're constantly stressed, your body is flooded with the hormone cortisol. This can throw your entire endocrine system out of whack, mess with progesterone levels, and ramp up inflammation.
A huge part of managing endometriosis naturally is tackling this mind-body connection head-on. By getting a handle on your body's stress response, you can directly influence your hormonal environment and quiet the inflammatory signals that fuel the pain cycle. It’s a powerful way to take back some control and find a sense of calm.
This doesn't mean you need to dedicate hours to meditation or completely reinvent your life. Small, consistent practices can make a world of difference in shifting your nervous system out of a constant state of high alert and into one of rest and healing.
Simple Ways to Dial Down Your Stress Response
Weaving stress management into your daily routine is all about finding what genuinely works for you. The key is to create small pockets of intentional calm that send a powerful "you are safe" signal to your body.
- Mindful Breathing: When you feel that wave of overwhelm, try the 4-7-8 breathing technique. It's simple: inhale through your nose for four seconds, hold for seven, and then exhale slowly through your mouth for eight. This one little exercise is incredibly effective at activating the parasympathetic nervous system, which is your body’s built-in relaxation trigger.
- Guided Mindfulness: Even just five to ten minutes a day can have a measurable impact on cortisol levels. Apps like Calm or Headspace have fantastic guided meditations designed specifically for pain management, which can help you learn to observe physical sensations without getting caught up in them.
- Journaling for Release: Pain can feel like it takes over everything. Taking a few minutes each day to just get your thoughts and feelings down on paper can be a huge relief. This process helps you externalize your worries, and you might even start to notice specific symptom triggers or patterns you'd otherwise miss.
A great starting point is to simply ask yourself, "What does my body need from me right now?" The answer might be a warm bath, a gentle stretch, or just five minutes of complete silence. The simple act of listening is the first step.
Making Restorative Sleep a Priority for Healing
For hormonal health, sleep isn't just a nice-to-have; it's absolutely critical. Yet, for so many with endometriosis, it's the first thing to go when pain flares up. It's during that deep, restorative sleep that your body does its most important repair work, regulates hormones, and processes the day's events. When you don't get enough of it, pain perception and inflammation can actually increase, making everything feel that much harder.
Creating a peaceful sleep sanctuary is one of the most important acts of self-care you can practice. It’s all about sending clear signals to your brain that it’s time to power down and prepare for deep rest, even when your body is feeling uncomfortable.
Think about making a few of these small adjustments to improve your sleep hygiene:
- Create a Wind-Down Ritual: About an hour before you plan to sleep, dim the lights and put away your phone, tablet, and laptop. The blue light from screens is notorious for suppressing melatonin, the hormone that tells your body it's time to sleep.
- Optimize Your Environment: Your bedroom should be a cave—cool, dark, and quiet. Blackout curtains can be a game-changer, and a white noise machine can do wonders for drowning out any disruptive sounds.
- Consider a Magnesium Supplement: Magnesium is often called the "relaxation mineral" for a reason. A specific form like magnesium glycinate, taken before bed, can help calm the nervous system and ease muscle tension, making it easier to drift off and stay asleep. Of course, you should always check with your doctor or healthcare provider before adding any new supplement to your routine.
Putting It All Together: Your Integrated Endometriosis Care Plan
Navigating endometriosis care can feel like trying to solve a complex puzzle with a million different pieces. But you've already done the hardest part: arming yourself with knowledge. Now, it's time to bring everything together—diet, movement, stress management, supplements—into a cohesive plan that truly works for you.
This isn't about choosing between natural therapies and conventional medicine. The most effective approach is an integrated one, blending the best of both worlds.
Think of yourself as the project manager of your own health. You're building a team that includes your doctor, a pelvic floor therapist, an acupuncturist, and most importantly, yourself. This collaborative model gives you a powerful support system and empowers you to make daily choices that lead to real, sustainable relief.
From Information to Action: Creating Your Framework
The goal is to move from simply knowing what to do to actually doing it. Trying to overhaul everything at once is a recipe for burnout. The key is to be strategic.
Start by picking a few key areas to focus on, track what happens, and build from there.
-
Become a Symptom Detective. Get a journal and start tracking everything. Note your pain levels on a scale of 1-10, your energy, bloating, mood, and other key symptoms. Log what you eat, how you move, and your stress levels. After a couple of cycles, you'll start seeing clear patterns emerge, revealing your unique triggers and what actually brings you relief.
-
Choose Your Starting Lineup. Look back at all the strategies we've discussed. Which one or two feel the most manageable right now? Maybe it’s just adding a handful of walnuts to your daily routine and committing to a 20-minute walk. It could be as simple as a 10-minute mindfulness practice before bed. Starting small is how you build momentum.
-
Prepare for Your Doctor’s Visit. Your medical team is your partner, not an adversary. Walk into your next appointment prepared. Bring your symptom journal and a clear, concise list of the natural approaches you’re interested in trying. This shows you're an engaged patient and opens the door for a much more productive conversation.
This process shifts you from being a passive recipient of care to an active participant. You're gathering your own data and using it to guide your journey.
Knowing Your Red Flags: When to Seek Medical Care
While these natural approaches are powerful tools for managing your day-to-day life, they are not a replacement for professional medical evaluation. Knowing when to call your doctor is a critical part of a safe and effective plan.
Crucial Takeaway: An integrated care plan is all about smart collaboration. Use natural therapies to manage daily symptoms and improve your quality of life, but always rely on your medical team for diagnosis, monitoring, and intervention when things change.
Be on high alert for these red flags and contact your doctor immediately if you experience any of them:
- Severe, Uncontrolled Pain: Pain that suddenly spikes, doesn't respond to your usual strategies, or feels completely debilitating.
- New or Worsening Bowel/Bladder Symptoms: This could be severe pain with bowel movements, rectal bleeding, or sudden difficulty urinating.
- High Fever with Pelvic Pain: This combination can be a sign of an infection that needs urgent attention.
- Unexplained Weight Loss: A significant and unintentional drop in weight should always be investigated.
The stress of living with chronic symptoms can create a vicious cycle, which is why a mind-body approach is so essential to any endometriosis plan.
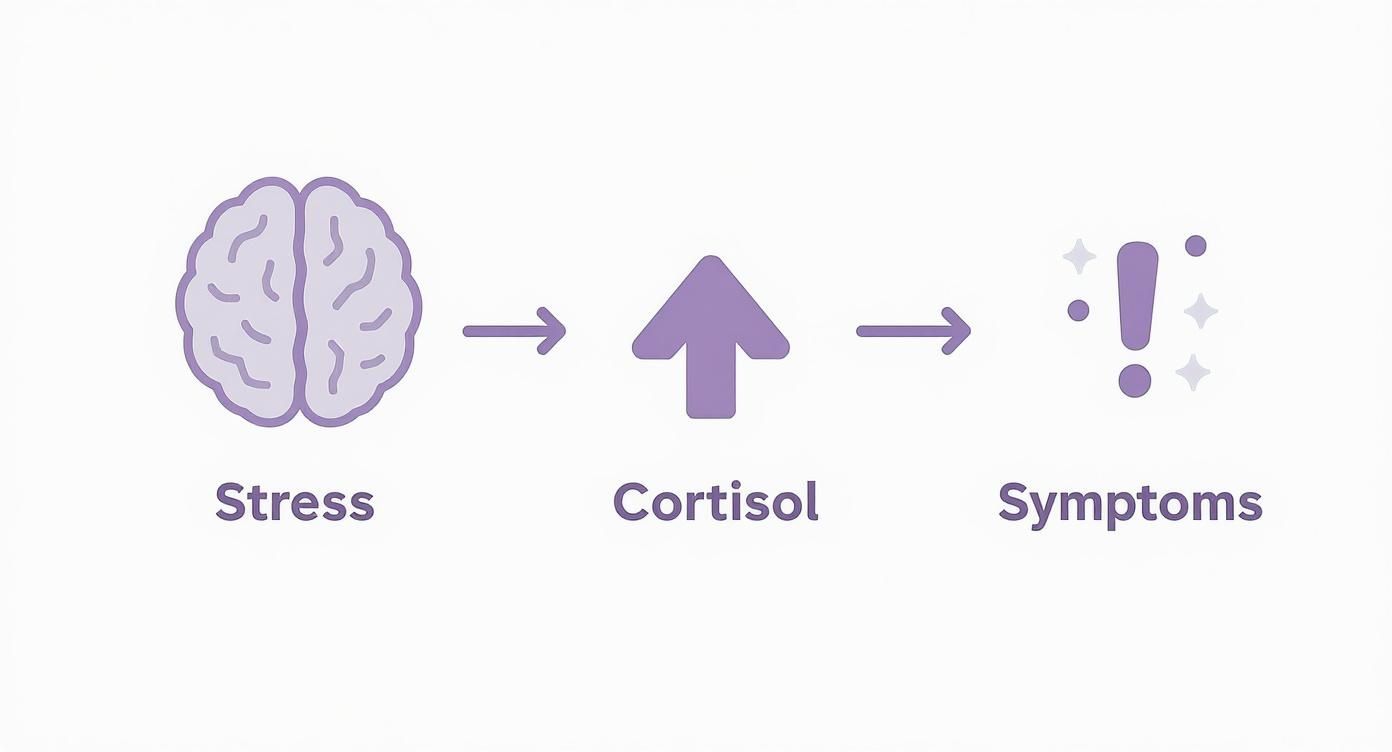
As this diagram shows, external stressors trigger a cortisol surge from the adrenal glands, which can amplify physical symptoms like pain and inflammation, creating a self-perpetuating loop.
Expanding Your Therapeutic Toolkit
Once you start feeling more confident and in control, you can begin to explore additional therapies. For instance, certain herbal medicines have shown real promise for hormonal regulation and pain relief.
A well-researched Japanese herbal formula, Tokishakuyakusan (TSS), has been shown in clinical studies to reduce inflammation and help balance hormones. In animal models, TSS treatment led to an incredible 60% reduction in the number of endometrial lesions and an 80% reduction in their total volume over several weeks. You can discover more insights about these endometriosis findings on Dovepress.com to dig into the science.
Building your plan is an ongoing, dynamic process. It's about listening to your body, making small adjustments, and celebrating every win. You have the power to create a life where you are in control of your endometriosis, not the other way around. This journey is about reclaiming your health, one intentional choice at a time.
At Eric Tsai Acupuncture and Herbs, we specialize in creating personalized, integrated care plans that combine the wisdom of Traditional Chinese Medicine with a modern understanding of conditions like endometriosis. If you are ready to build a supportive team and find lasting relief, we invite you to book a consultation with Dr. Eric Tsai today.